Understanding Urinary Tract Infections and Spasms
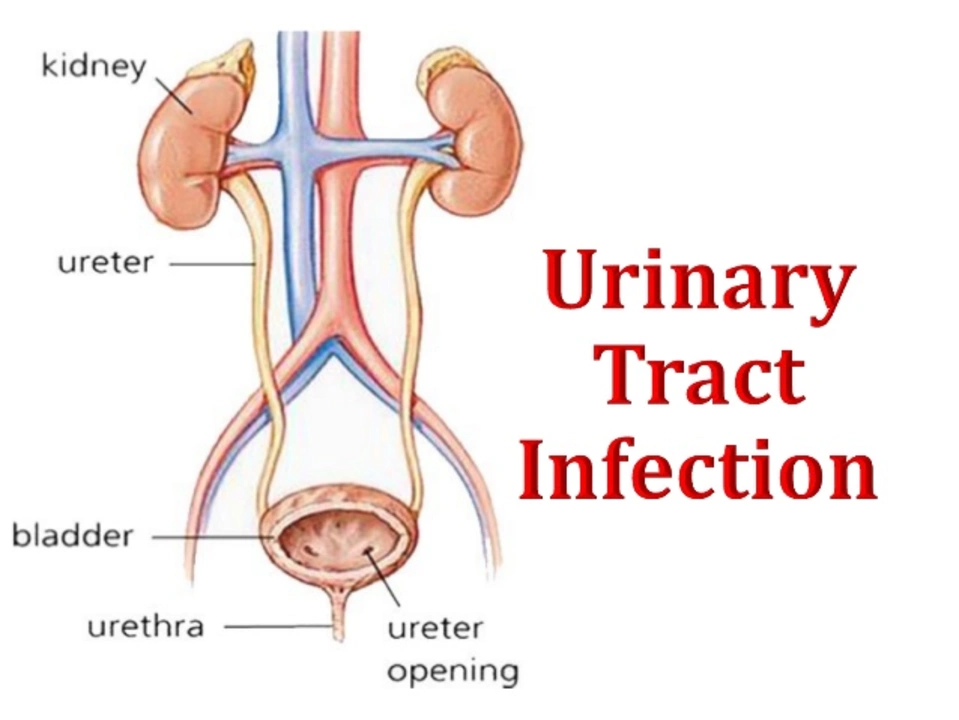
Urinary tract infections (UTIs) are a common issue that affects millions of people each year. They occur when bacteria enter the urinary tract and cause inflammation, leading to symptoms such as burning during urination, frequent urges to urinate, and even spasms in the bladder or pelvic area. In this article, we'll take a closer look at the relationship between UTIs and spasms and discuss ways to prevent and treat these conditions.
Causes and Symptoms of Urinary Tract Infections
Urinary tract infections are typically caused by bacteria, most often Escherichia coli (E. coli), which normally lives in the intestines. These bacteria can enter the urinary tract through the urethra and travel up into the bladder, causing an infection. This can lead to a variety of symptoms, such as:
- Pain or burning during urination
- A strong, persistent urge to urinate
- Cloudy, dark, bloody, or strong-smelling urine
- Feeling tired or shaky
- Lower abdominal pain or pressure
It's important to note that not everyone with a UTI will experience all of these symptoms, and some people may not have any symptoms at all.
How UTIs Lead to Spasms
When a UTI occurs, the inflammation and irritation caused by the infection can lead to involuntary muscle contractions in the bladder and pelvic area, resulting in spasms. These spasms can be quite painful and uncomfortable, and they may also make it difficult to empty the bladder completely. This can further exacerbate the infection, as stagnant urine in the bladder can provide a breeding ground for bacteria to multiply.
Additionally, the pain and discomfort caused by spasms can lead to a cycle of anxiety and tension, which can make the spasms even worse. This is why it's crucial to address both the infection and the spasms in order to find relief.
Treatment Options for UTIs and Spasms
If you suspect you have a urinary tract infection, it's important to see a healthcare professional for proper diagnosis and treatment. They will likely prescribe antibiotics to kill the bacteria causing the infection. In addition to antibiotics, there are several other treatment options that can help alleviate spasms and other UTI symptoms:
- Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help reduce pain and inflammation
- Heating pads or warm baths can provide relief from spasms and soothe the pelvic area
- Drinking plenty of water can help flush bacteria from the urinary tract and dilute urine, making it less irritating to the bladder
- Avoiding caffeine, alcohol, and spicy foods, which can irritate the bladder and worsen symptoms
It's important to follow your healthcare provider's recommendations and complete the full course of antibiotics, even if you start to feel better before the medication is finished. This ensures that the bacteria are completely eliminated and helps prevent the infection from returning.
Preventing UTIs and Spasms
While it may not be possible to completely prevent urinary tract infections, there are several steps you can take to reduce your risk and minimize the likelihood of experiencing spasms:
- Drink plenty of water each day to help flush bacteria from your urinary tract
- Wipe from front to back after using the restroom to prevent bacteria from spreading from the anus to the urethra
- Urinate frequently, and avoid holding in urine for long periods of time
- Avoid using douches, scented feminine hygiene products, and harsh soaps, which can irritate the urethra and increase the risk of infection
- Wear loose, breathable clothing and underwear made from natural fibers, such as cotton, to prevent moisture buildup and bacterial growth
By following these steps, you can help maintain a healthy urinary tract and reduce your risk of developing UTIs and spasms.
When to Seek Medical Help
If you're experiencing symptoms of a urinary tract infection or spasms, it's essential to consult a healthcare professional for proper diagnosis and treatment. Don't hesitate to seek help if you have:
- Severe pain or discomfort that doesn't improve with over-the-counter pain relievers
- Fever or chills, which can be a sign of a more serious infection
- Blood in your urine
- Difficulty urinating or a complete inability to urinate
By seeking prompt medical attention, you can ensure that you receive the appropriate treatment and prevent complications from UTIs and spasms.

Comments
Justin Scherer
Staying hydrated is the easiest way to keep bacteria from hanging out in your bladder, so aim for at least eight glasses of water a day.
April 30, 2023 AT 05:45
Pamela Clark
Oh joy, another “essential guide” reminding us to pee more often – because we clearly needed a reminder from the internet.
May 3, 2023 AT 17:05
Diane Holding
Wiping front to back after using the bathroom cuts down the chance of transferring gut bacteria to the urethra.
May 7, 2023 AT 04:25
Cheyanne Moxley
Honestly, we all have to take responsibility for our own hygiene habits; blaming the world for a preventable UTI is just lazy.
May 8, 2023 AT 08:12
Kevin Stratton
The relationship between urinary infections and muscle spasms is a vivid illustration of how microbes can influence our nervous system.
When bacteria colonize the urinary tract they release toxins that irritate the lining of the bladder.
This irritation triggers afferent nerve fibers to fire, sending pain signals to the spinal cord.
In response, the detrusor muscle can contract erratically, producing the spasms described in the article.
Moreover, the inflammatory cascade releases cytokines that sensitize nearby sensory neurons.
Sensitized neurons lower the threshold for muscle activation, meaning even mild bladder filling can provoke a spasm.
The mind‑body connection also plays a role; anxiety about pain can increase sympathetic tone, which further tightens pelvic muscles.
From a microbiological perspective, Escherichia coli is adept at exploiting the urinary mucosa, creating a micro‑environment conducive to persistent irritation.
Recurrent infections can remodel the bladder’s muscular architecture, leading to chronic hyper‑responsiveness.
Treatment, therefore, isn’t just about killing the bacteria but also about breaking the feedback loop.
Anti‑inflammatory agents can dampen cytokine activity, while gentle pelvic floor physiotherapy can retrain muscle patterns.
Hydration remains a cornerstone because dilute urine reduces toxin concentration and mechanical stress on the bladder wall.
Dietary modifiers like avoiding caffeine and spicy foods lower irritant load, preventing secondary spasm triggers.
In practice, a multidisciplinary approach that combines antibiotics, pain management, and behavioral therapy yields the best outcomes.
Ultimately, understanding the cascade from microbial invasion to muscular response empowers patients to take proactive steps toward recovery.
May 11, 2023 AT 19:32
Manish Verma
While your deep‑dive is interesting, most readers just want a quick fix, not a lecture on cytokines-keep it simple.
May 15, 2023 AT 06:52
Lionel du Plessis
UTI pathogenesis involves E.coli ascend via urethra colonize bladder leading to inflammation and overactive detrusor muscle spasms
May 18, 2023 AT 18:12
Andrae Powel
Antibiotics clear the infection, but finishing the full course prevents resistant strains; combine that with ibuprofen for pain and a heating pad for muscle relief.
May 22, 2023 AT 05:32
Leanne Henderson
Exactly! Adding a warm compress really helps the pelvic muscles relax and reduces the spasm intensity-great tip! :)
May 23, 2023 AT 09:18
Megan Dicochea
Drinking water is key it flushes out bacteria but also remember to urinate after sex it helps clear any introduced microbes also avoid tight clothing
May 26, 2023 AT 20:38
Jennie Smith
Think of your bladder like a tiny garden-water it, keep the weeds (bacteria) out, and it’ll flourish without those pesky “spasm” storms.
May 30, 2023 AT 07:58
Greg Galivan
Stop ignoring the symptoms, u need to see a doc now or u’ll end up with a chronic infection.
June 2, 2023 AT 19:18
Anurag Ranjan
Probiotics can rebalance gut flora, reducing the chance of E.coli migrating to the urinary tract.
June 6, 2023 AT 06:38
James Doyle
From a urological standpoint, the pathophysiology of infection‑induced detrusor overactivity hinges upon urothelial receptor up‑regulation and subsequent cholinergic hyperstimulation. Clinicians frequently observe that nitrofurantoin, whilst effective in eradicating gram‑negative bacilli, may not fully attenuate the associated neurogenic reflex arc. Therefore, adjunctive anticholinergic therapy, such as oxybutynin, is often prescribed to mitigate involuntary contractions. It is also prudent to assess for comorbidities like diabetes mellitus, which can exacerbate autonomic dysfunction and predispose patients to recurrent episodes. Comprehensive patient education on behavioral modifications-fluid intake optimization, timed voiding, and pelvic floor biofeedback-constitutes an integral component of long‑term management. In cases of refractory spasms, intravesical Botulinum toxin injections have demonstrated efficacy in reducing detrusor pressure. Ultimately, a multimodal regimen that synergistically addresses microbial eradication, neuromuscular control, and lifestyle factors yields the most favorable prognosis.
June 9, 2023 AT 17:58
Edward Brown
What they don't tell you is that the over‑prescription of antibiotics fuels resistant super‑bugs, turning a simple UTI into a covert bio‑weapon against the public.
June 13, 2023 AT 05:18
ALBERT HENDERSHOT JR.
It is commendable that you are seeking evidence‑based strategies; maintaining hydration, adhering to prescribed antibiotics, and incorporating pelvic floor exercises will collectively promote recovery 😊.
June 16, 2023 AT 16:38
Suzanne Carawan
Because we all needed another lecture on pee hygiene.
June 20, 2023 AT 03:58
Kala Rani
Honestly, most of this advice is just common sense disguised as expert advice.
June 23, 2023 AT 15:18