Understanding Sexually Transmitted Infections
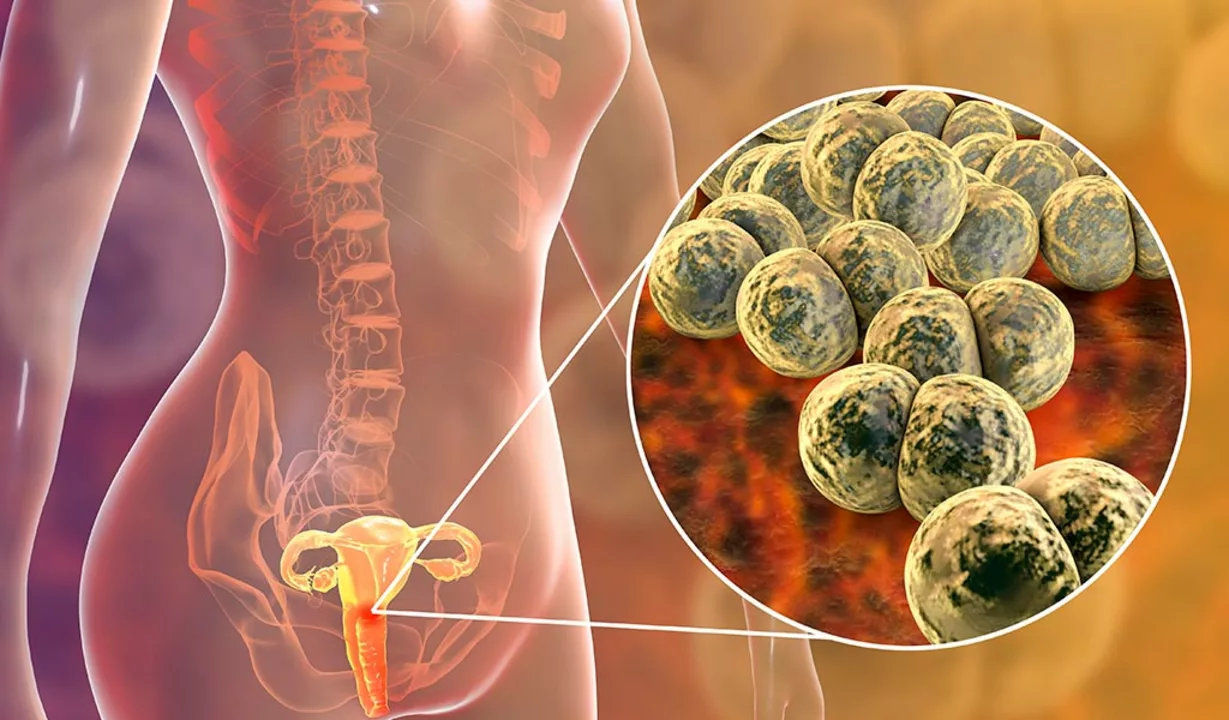
Before diving into the connection between sexually transmitted infections (STIs) and infertility, it is essential to understand what STIs are and how they are transmitted. Sexually transmitted infections, also known as sexually transmitted diseases or STDs, are infections that spread through sexual contact. They can be caused by various microorganisms, including bacteria, viruses, and parasites.
Common STIs include chlamydia, gonorrhea, syphilis, human papillomavirus (HPV), genital herpes, and human immunodeficiency virus (HIV). These infections can cause a wide range of symptoms, from mild discomfort to severe complications if left untreated.
How STIs Lead to Infertility
Sexually transmitted infections can cause damage to the reproductive system, which may result in infertility. Infertility is defined as the inability to conceive after a year of regular, unprotected sex. Both men and women can be affected by STI-induced infertility, and the specific cause can vary depending on the infection. The most common STIs linked to infertility are chlamydia and gonorrhea.
These infections can cause inflammation in the reproductive organs, leading to scarring and blockages. In women, this may result in blocked fallopian tubes, preventing the sperm from reaching the egg. In men, it can cause blockages in the sperm-carrying tubes, reducing sperm count and mobility.
Pelvic Inflammatory Disease and Infertility
Pelvic inflammatory disease (PID) is a common complication of untreated chlamydia and gonorrhea infections in women. PID is an infection of the female reproductive organs, including the uterus, fallopian tubes, and ovaries. It occurs when bacteria from an STI or other source spread from the vagina to the upper reproductive tract.
Untreated PID can cause scarring and damage to the fallopian tubes, increasing the risk of ectopic pregnancy and infertility. Ectopic pregnancy is a life-threatening condition where a fertilized egg implants outside the uterus, usually in the fallopian tube. It is crucial to recognize and treat PID early to avoid long-term complications.
Male Infertility and STIs
Men can also experience infertility due to sexually transmitted infections. Infections like chlamydia and gonorrhea can cause inflammation in the epididymis, a coiled tube that stores and carries sperm. This inflammation, known as epididymitis, can lead to blockages and reduced sperm function, making it harder to fertilize an egg.
Additionally, some viral STIs, such as HIV and genital herpes, can directly affect sperm quality and quantity, further decreasing fertility. Early detection and treatment are crucial in minimizing the impact of STIs on male fertility.
Preventing STI-related Infertility
Preventing STI-related infertility starts with practicing safe sex and maintaining good sexual health. Regular STI testing is essential, especially for those with multiple sexual partners or those in non-monogamous relationships. Early detection and treatment of STIs can reduce the risk of complications and infertility.
Using barrier methods, such as condoms, during sex can help protect against STIs. Additionally, getting vaccinated against certain infections, like HPV and hepatitis B, can further reduce the risk of contracting these infections and their associated complications.
Treatment Options for STI-related Infertility
If you are diagnosed with an STI and are concerned about infertility, it is essential to speak with a healthcare professional. They can help determine the best course of treatment and provide guidance on next steps. For bacterial STIs like chlamydia and gonorrhea, antibiotics are often prescribed to clear the infection.
For those already experiencing infertility due to an STI, fertility treatments may be necessary. In vitro fertilization (IVF), intrauterine insemination (IUI), and surgery to correct blockages are some of the options available to help couples conceive.
The Importance of Sexual Health Education
Understanding the connection between sexually transmitted infections and infertility highlights the importance of sexual health education. Early and comprehensive education about STIs, safe sex practices, and the potential consequences of untreated infections can help individuals make informed decisions about their sexual health.
Sexual health education should be accessible, age-appropriate, and inclusive, providing accurate information to help individuals protect themselves and their partners. By promoting awareness and understanding of STIs and their potential impact on fertility, we can work towards reducing the prevalence of these infections and their associated complications.

Comments
Kala Rani
STIs aren’t the only reason people face infertility yeah
May 12, 2023 AT 11:17
Donal Hinely
Yo, this post is spot on about the dangers of untreated chlamydia and gonorrhea – they can wreck your reproductive system faster than you can say ‘condom’. But let’s not forget that cultural attitudes toward sex education still suck in many places, so people keep getting caught off‑guard. Use protection, get tested, and stop the stigma, bro. Otherwise you’re just feeding the cycle of infertility.
May 13, 2023 AT 19:46
christine badilla
Omg, reading this gave me chills! It’s like a tragic soap‑opera where the villain is a silent infection screwing up dreams of babies. Seriously, if you ignore those symptoms you’re signing up for heartbreak.
May 14, 2023 AT 23:33
Octavia Clahar
Look, I get the drama but the facts are plain – untreated STIs are a real roadblock. Let’s keep the conversation friendly yet honest so nobody gets misled.
May 16, 2023 AT 03:20
eko lennon
The cascade of physiological events triggered by an undiagnosed STI is nothing short of a domino effect that can culminate in irreversible infertility.
When chlamydia ascends from the lower genital tract, it incites a robust inflammatory response in the fallopian tubes.
This inflammation recruits neutrophils and macrophages, which release matrix metalloproteinases that degrade the extracellular matrix.
Consequently, fibrotic scar tissue forms, narrowing the tubal lumen and obstructing gamete passage.
In men, analogous pathogen‑induced epididymitis triggers edema, which compresses the ductal epithelium.
Prolonged edema compromises spermatogenesis, leading to oligospermia and diminished motility.
Virally mediated infections, like HIV, can alter seminal plasma composition, reducing antioxidant capacity and sperm viability.
Moreover, the psychosocial stress of a chronic STD diagnosis often leads to delayed medical consultation, exacerbating tissue damage.
Clinical guidelines underscore the importance of early antimicrobial therapy to halt this cascade before scarring becomes permanent.
Yet, real‑world barriers-stigma, lack of access, and misinformation-impede timely treatment.
Vaccination against HPV and hepatitis B represents a prophylactic strategy that can curtail the incidence of infection‑related infertility.
Screening protocols, especially in high‑risk populations, must be integrated into routine primary care visits.
When structural damage is already present, assisted reproductive technologies such as IVF become viable recourse, albeit at significant cost.
Surgeons can perform tubal anastomosis or reconstructive procedures, but success rates vary depending on scar severity.
Ultimately, comprehensive sexual health education, coupled with accessible diagnostic services, remains the cornerstone of infertility prevention.
May 17, 2023 AT 07:06
Sunita Basnet
Great insights! Let’s amplify preventive care using evidence‑based protocols and dynamic outreach. Early detection, rapid antimicrobial stewardship, and robust immunization pipelines can mitigate downstream reproductive sequelae.
May 18, 2023 AT 10:53
Melody Barton
Exactly – act now, get tested, and push for widespread education. No more excuses, protect your future families.
May 19, 2023 AT 14:40
Justin Scherer
Appreciate the supportive tone. It’s vital that we keep the dialogue inclusive so everyone feels empowered to seek help.
May 20, 2023 AT 18:26