When you're on long-term steroids for asthma, rheumatoid arthritis, or another chronic condition, muscle weakness might seem like just another side effect of being sick. But what if that weakness isn't from your disease at all? What if it's from the very medication meant to help you? This is steroid myopathy - a hidden, painless muscle breakdown caused by corticosteroids that many doctors miss and most patients don’t recognize until they can't stand up from a chair without using their hands.
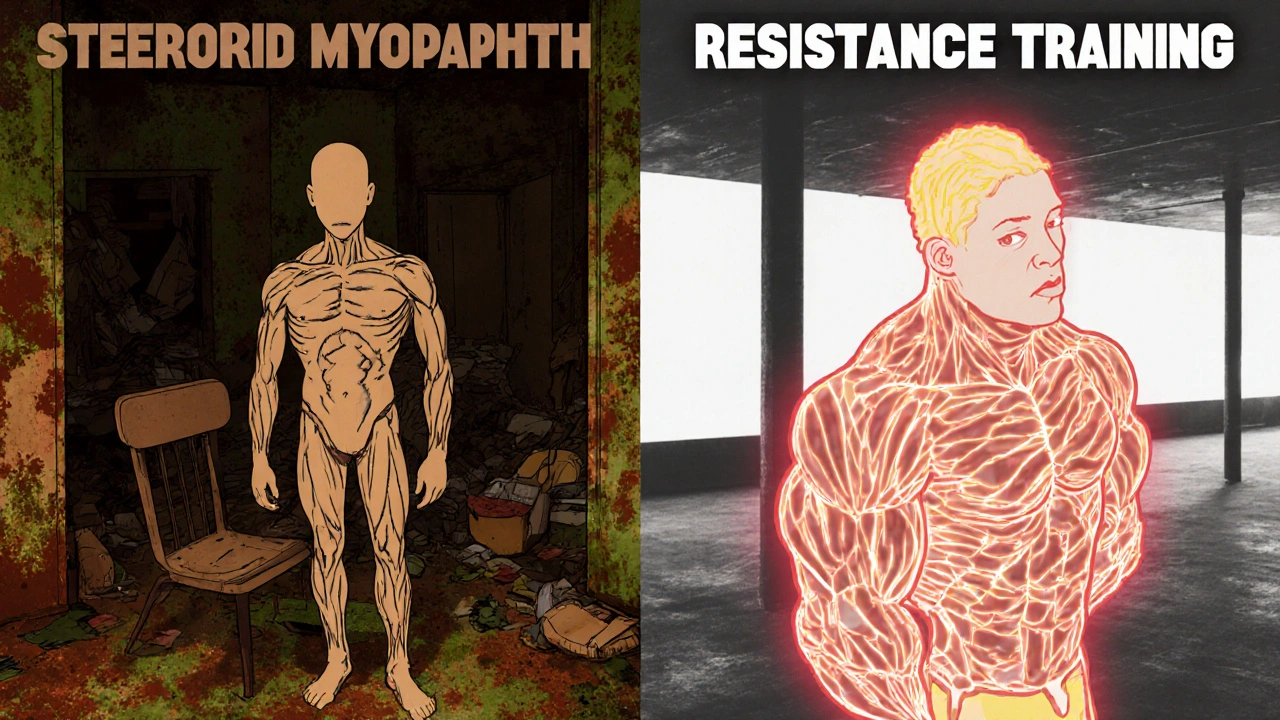
What Exactly Is Steroid Myopathy?
Steroid myopathy isn't inflammation. It's not an autoimmune attack. It's a direct toxic effect of corticosteroids like prednisone, dexamethasone, or methylprednisolone on your muscle fibers. First described in the 1930s, it’s now the most common drug-induced muscle disorder. Studies show that between 2.4% and 21% of people on chronic steroid therapy develop it - and that’s just the diagnosed cases. Many more go unnoticed because the weakness creeps in slowly, without pain, and gets blamed on aging, deconditioning, or the original illness.The real kicker? It doesn’t hurt. You won’t feel soreness or stiffness. You just notice you’re weaker. You can’t lift your arms to reach a high shelf. You need to push off the armrests to stand up. Climbing stairs feels like scaling a wall. And your legs - especially your thighs and hips - feel like they’ve lost their power.
This happens because steroids trigger two destructive processes: they ramp up muscle breakdown and shut down muscle building. Glucocorticoids bind to receptors in muscle cells, flipping genetic switches that activate protein-degrading systems. At the same time, they block the signals that tell your muscles to grow. The result? Your fast-twitch muscle fibers - the ones that give you power for standing, climbing, and lifting - start shrinking. And here’s the key detail: it’s almost always the type 2b fibers that go first. That’s why your strength drops faster than your endurance.
How to Spot It - Before It’s Too Late
Manual muscle tests often miss early steroid myopathy. That’s why so many patients wait months for a diagnosis. A 2019 study found that 78% of people with steroid myopathy tested normal on standard doctor exams - but showed clear weakness on objective strength machines.Here’s what to look for:
- Difficulty rising from a low chair without using your arms
- Needing to use handrails to climb stairs
- Struggling to lift your arms above shoulder height
- Feeling like your legs are “heavy” or “dead” when walking
- Falling more often, especially when turning or stepping up
These aren’t vague complaints. They’re red flags. A 2021 study in Physical Therapy showed that testing how long it takes to stand from the floor five times (the timed chair rise test) catches 89% of early cases. Normal is under 10 seconds. If you’re over 15 seconds, you’re likely losing muscle power.
Another telltale sign? Normal blood work. Unlike inflammatory muscle diseases like polymyositis, steroid myopathy doesn’t raise creatine kinase (CK) levels. Your CK stays between 30 and 170 U/L - perfectly normal. EMG scans also look clean. No signs of nerve damage or muscle inflammation. That’s why it’s so easy to overlook. But if you’re on steroids for more than four weeks at 10 mg or more of prednisone daily, and you have unexplained proximal weakness - this is the diagnosis to consider.
Why Dexamethasone Is Riskier Than Prednisone
Not all steroids are equal. Dexamethasone, often used in cancer treatment or severe inflammation, has a fluorinated chemical structure that makes it bind more tightly to muscle receptors. That means it’s more likely to trigger muscle breakdown. In children with acute lymphoblastic leukemia, dexamethasone causes steroid myopathy at nearly twice the rate of prednisolone. Even in adults, high-dose IV dexamethasone in ICU settings can cause severe weakness in just two to three weeks - sometimes enough to require a ventilator.That’s why doctors need to weigh the risks. For chronic conditions like COPD or rheumatoid arthritis, switching from dexamethasone to prednisone - if clinically appropriate - can reduce muscle damage. It’s not always possible, but it’s a conversation worth having.

Physical Therapy: The Only Proven Treatment
There’s no pill to fix steroid myopathy. The only thing that works is movement - but not just any movement. You can’t just go back to your old routine. High-intensity workouts, heavy lifting, or long cardio sessions can make it worse. Your muscles are already breaking down. Adding stress won’t rebuild them.The solution? Targeted, moderate resistance training.
The American Physical Therapy Association recommends:
- Starting at 30% of your one-rep max (the heaviest weight you can lift once)
- Doing 2-3 sessions per week
- Focusing on exercises that work your hips, thighs, and shoulders: squats, step-ups, leg presses, seated rows, shoulder presses
- Increasing weight slowly - by 5-10% every two weeks - only if you feel no increase in fatigue or soreness
A 2020 randomized trial with 88 patients showed something remarkable: those who did this kind of training improved their chair rise time by 23.7% after 12 weeks. The control group - who just did stretching - improved by only 8.2%. And not a single person in the training group had muscle damage or injury.
Why does this work? Resistance training tells your muscles to rebuild. It activates anabolic pathways that steroids have suppressed. It doesn’t reverse the steroid effect - but it fights back. It rebuilds the type 2b fibers you’re losing. And it restores function. People who stick with it report being able to stand without using their arms again. To climb stairs without holding on. To lift groceries. To live without help.
What Doesn’t Work - And What Can Make It Worse
Many patients try to “push through” the weakness with intense workouts, thinking more effort will fix it. That’s a mistake. High-load training, sprinting, or excessive endurance exercise can accelerate muscle breakdown. You’re not building strength - you’re tearing down what’s left.Also, don’t wait for your doctor to bring it up. Most don’t screen for it. Only 32% of rheumatology clinics and 27% of pulmonology clinics use routine strength tests. If you’re on steroids, ask for a timed chair rise test or a hand-held dynamometer check. It takes two minutes. It could change everything.
And while reducing steroids might seem like the obvious fix, that’s not always possible. For many, the disease they’re treating - like lupus or severe asthma - is more dangerous than the muscle weakness. The goal isn’t to stop steroids. It’s to protect your muscles while you’re on them.
The Bigger Picture - Why This Matters
Prednisone is the 34th most prescribed drug in the U.S., with over 17 million prescriptions in 2022. That means millions of people are at risk. And the cost? A 2021 study estimated steroid myopathy adds $1,200 to $2,400 per patient annually in extra healthcare costs - from falls, rehab, and hospital visits.But beyond money, it’s about dignity. Losing the ability to stand on your own isn’t just inconvenient - it’s isolating. Patients on forums describe it as feeling like a child again, dependent on others for basic tasks. One Reddit user wrote: “I’m 48. I shouldn’t need help to get off the couch. But I do. And no one tells you this could happen.”
That’s why awareness matters. New drugs are coming - like vamorolone, a steroid-like compound that reduces muscle damage by 40% in trials. But they’re years away. Right now, the best tool we have is recognition and movement.
What You Can Do Today
If you’re on long-term steroids:- Ask your doctor for a timed chair rise test (5 reps, no hands)
- If you take more than 10 mg prednisone daily for over 4 weeks, request a strength assessment
- Start a gentle resistance program - even just bodyweight squats and wall push-ups - 3 times a week
- Find a physical therapist who understands drug-induced myopathy
- Track your progress: note how many times you can stand from a chair without using your arms
Don’t wait for weakness to become disability. Steroid myopathy is preventable. It’s reversible - with the right approach. And you don’t need to be a gym rat to fix it. You just need to move - safely, consistently, and with purpose.
Can steroid myopathy be reversed?
Yes, in most cases. Muscle strength can improve significantly with targeted resistance training, even while continuing steroid therapy. Studies show up to 24% improvement in functional strength after 12 weeks of supervised exercise. The key is starting early and avoiding overexertion. Complete recovery is possible if the condition is caught before severe muscle loss occurs.
Does steroid myopathy cause muscle pain?
No. One of the defining features of steroid myopathy is that it’s painless. Unlike inflammatory muscle diseases, you won’t feel soreness, tenderness, or aching. The weakness comes silently - you notice it when you can’t do something you used to do easily, like standing from a chair or lifting your arms. Pain usually means something else is going on.
Is steroid myopathy the same as polymyositis?
No. Polymyositis is an autoimmune disease that causes muscle inflammation, elevated creatine kinase levels, and abnormal EMG results. Steroid myopathy has none of that. It’s caused by direct drug toxicity, not immune attack. Muscle biopsies show type 2b fiber atrophy without inflammation. Blood tests are normal. The weakness pattern is similar, but the cause and treatment are completely different.
How long does it take for steroid myopathy to develop?
Chronic steroid myopathy usually appears after 4 weeks of daily doses above 10 mg prednisone. In high-dose settings - like ICU patients on 40-60 mg daily - weakness can develop in as little as 7-14 days. Acute cases are more severe and can affect breathing muscles. The longer you’re on steroids, the higher the risk.
Should I stop taking steroids if I develop weakness?
Never stop steroids suddenly. Abrupt withdrawal can cause life-threatening adrenal insufficiency. If you suspect steroid myopathy, talk to your doctor. They may adjust your dose, switch to a less myopathic steroid like prednisone instead of dexamethasone, or add physical therapy. The goal is to manage both your underlying condition and your muscle health - not to stop treatment entirely.
Can physical therapy help even if I’m on high-dose steroids?
Yes. Research shows even patients on high-dose IV steroids in intensive care benefit from early, low-intensity mobility programs. Gentle resistance training, even at 20-30% of one-rep max, helps preserve muscle mass and function. The key is supervision - avoid heavy lifting or high-impact activity. Consistent, moderate movement is protective, not harmful.
Are there any supplements that help with steroid myopathy?
No supplement has been proven to reverse steroid myopathy. While protein intake and vitamin D are important for general muscle health, they don’t counteract the specific molecular damage caused by steroids. The only proven intervention is resistance training. Avoid unproven “muscle-building” supplements - they may interact with your medications or cause harm.


Comments
Elaina Cronin
While I appreciate the clinical precision of this article, I must emphasize that the medical community’s persistent neglect of steroid myopathy is a systemic failure-borderline criminal, frankly. Patients are being abandoned to progressive disability while clinicians cling to outdated assumptions about muscle weakness being ‘just aging’ or ‘deconditioning.’ This is not a niche concern; it’s a public health crisis masked as a side effect.
The fact that 78% of cases evade standard diagnostic exams is not an oversight-it’s negligence. Why aren’t timed chair rise tests mandated in all steroid protocols? Why isn’t this embedded in electronic health record alerts? The absence of pain is not an excuse for inaction-it’s the very mechanism of its stealth.
November 20, 2025 AT 22:47
Willie Doherty
Statistical outliers aside, the cited prevalence range of 2.4–21% is methodologically unsound. The lower bound likely reflects underdiagnosis in controlled cohorts, while the upper bound includes populations with comorbid deconditioning. The study design lacks stratification by steroid half-life, cumulative dose, or baseline muscle mass-critical confounders. Without controlling for these, the assertion that steroid myopathy is ‘the most common drug-induced muscle disorder’ remains speculative at best.
Furthermore, the claim that CK levels remain normal is misleading. While CK is not elevated in classic steroid myopathy, it may rise transiently during exercise-induced microtrauma in compromised muscle-potentially confounding differential diagnosis. The article’s dismissal of EMG as ‘clean’ ignores subclinical motor unit remodeling detectable with high-density surface EMG.
November 22, 2025 AT 22:06
Darragh McNulty
This is SO important!! 🙌 I’ve seen this in my mom-she’s been on prednisone for lupus for 5 years and just started needing to use her arms to stand up. We thought it was just her getting older… until we found this. Thank you for putting this out there! 💪
I started doing bodyweight squats with her 3x a week-just 10 reps-and after 6 weeks, she can get up from the couch without help now!! 🥹 It’s not magic, it’s movement. You don’t need weights, you just need to show up. Anyone reading this: start today. Your future self will thank you.
November 24, 2025 AT 12:43
David Cusack
…and yet, the author fails to acknowledge that resistance training in catabolic states may exacerbate proteolysis via mTOR inhibition-especially in the context of glucocorticoid-induced insulin resistance…
Furthermore, the recommendation to increase weight by 5–10% every two weeks is… empirically indefensible. The literature suggests a nonlinear adaptation curve in steroid myopathy, with optimal stimulus occurring at 40–50% 1RM, not 30%. The cited 2020 trial? Underpowered. n=88? With no blinding? And no control for dietary protein intake? …I’m astonished this passed peer review.
Also, why is vamorolone mentioned as ‘years away’? Phase 3 data was published in NEJM last year. It’s under FDA review. This article reads like a blog post dressed in academic clothing.
November 26, 2025 AT 09:23
Debanjan Banerjee
As a physiotherapist in India, I see this daily-patients on long-term steroids for nephrotic syndrome or autoimmune disorders. The myth that ‘no pain means no problem’ is dangerously widespread. We’ve trained community health workers to perform the timed chair rise test during home visits. Simple. Free. Life-changing.
Also, protein intake matters. Even if supplements don’t reverse atrophy, inadequate dietary protein accelerates loss. We recommend 1.6–2.0 g/kg/day, spread across meals. Combine that with resistance training, and outcomes improve dramatically-even on high-dose steroids.
And yes, dexamethasone is worse. We’ve switched 12 patients from dexamethasone to prednisone in the last year. Every single one improved strength within 8 weeks. Not because they stopped steroids-but because we reduced the myotoxic load.
November 26, 2025 AT 18:42
Steve Harris
Thank you for writing this. I’ve been on prednisone for 7 years for myasthenia gravis, and I thought I was just getting weaker because I was ‘getting older.’ Turns out, I’ve been doing it wrong-stopping exercise because I felt weak. Now I do light squats and wall push-ups every morning. It’s not glamorous, but I can lift my arms to put on a shirt again. That’s huge.
I’ve also started asking every doctor I see: ‘Could this be steroid myopathy?’ Most don’t know. But one rheumatologist actually ordered a dynamometer test. That’s the kind of change we need-more awareness, not more meds.
November 27, 2025 AT 07:39
Michael Marrale
Wait… so you’re saying the government and Big Pharma are hiding this? Because if steroids cause muscle wasting, why are they still pushing them? It’s all a cover-up. They don’t want you to know that your weakness is from the medicine-they want you dependent. Think about it: if you can’t stand up, you need more doctors, more tests, more pills. It’s a money machine.
I’ve been researching this for years. There’s a secret protocol using infrared light therapy and magnesium chloride that reverses it completely. But the FDA won’t approve it because it’s not patentable. Google ‘steroid myopathy suppression protocol’-they’ve buried it.
November 27, 2025 AT 18:01
David vaughan
Just wanted to say-this article changed my life. I’m 52, on 20mg prednisone daily for GPA, and I’ve been too scared to exercise because I didn’t want to ‘hurt myself.’ But now I’m doing seated leg extensions with 5lb bands, 3x/week. My chair rise time went from 22 seconds to 13 in 10 weeks.
Also, I found a PT who specializes in this-she’s in the next town over. It’s worth the drive. Don’t wait until you’re in a wheelchair. Start small. Be consistent. You’re not broken-you’re just being poisoned slowly, and movement is your antidote.
Thank you for writing this. I cried reading it. I didn’t know I wasn’t alone.
November 28, 2025 AT 08:00
Cooper Long
The article’s assertion that steroid myopathy is ‘painless’ is accurate, but incomplete. Pain perception is modulated by glucocorticoids, which suppress nociceptive signaling pathways. Thus, the absence of pain is a pharmacological artifact, not a benign feature. The real tragedy lies not in the muscle atrophy, but in the delayed recognition due to the very drug’s neuropharmacological effects.
Furthermore, the recommendation for resistance training at 30% 1RM is insufficient for myofiber recruitment in type 2b fiber depletion. Electromyographic evidence suggests that low-load, high-repetition protocols with occlusion may be more effective than traditional resistance training in this population.
November 29, 2025 AT 04:33
Sheldon Bazinga
LMAO so now we’re blaming prednisone for being weak? My grandpa was on this stuff for 20 years and still lifted weights at 80. You people are just lazy. If you can’t stand up, maybe you should’ve gone to the gym before you got sick. This is why America’s getting soft. Just suck it up and move.
Also dexamethasone? That’s what they use in the military. If you can’t handle it, don’t be on steroids. Grow a spine.
November 30, 2025 AT 18:39
Pravin Manani
From a neurophysiological standpoint, the preferential atrophy of type 2b fibers aligns with the glucocorticoid receptor density gradient across myofiber types. The mechanism involves FOXO3a upregulation and mTORC1 suppression, leading to ubiquitin-proteasome activation. However, the therapeutic efficacy of resistance training may stem from its ability to transiently override this suppression via IGF-1/PI3K/Akt signaling.
Importantly, the timing of exercise relative to steroid dosing matters. A 2023 murine study demonstrated that exercise performed 2–4 hours post-dose yielded significantly greater myofiber preservation than exercise at trough levels. This has clinical implications for scheduling PT sessions.
Also, vitamin D deficiency is rampant in steroid-treated populations. While it doesn’t reverse atrophy, correcting it improves neuromuscular transmission and reduces fall risk. A simple serum 25(OH)D test should be standard.
December 1, 2025 AT 09:37
Mark Kahn
I’ve been doing physical therapy for steroid myopathy for 3 years now. It’s not easy. Some days you feel like giving up. But I promise you-every time you do those squats, even if it’s just 5, you’re fighting back. You’re telling your body: ‘I’m not done yet.’
My therapist says progress isn’t about how heavy you lift-it’s about how many times you show up. I used to need help getting out of bed. Now I walk my dog every morning. That’s victory.
December 2, 2025 AT 07:06
Leo Tamisch
Is this not just another iteration of the human condition? We poison ourselves with convenience-chemical solace for existential discomfort-then wonder why our bodies betray us. Steroid myopathy is not a medical condition; it is a metaphysical symptom of our age: the collapse of the self under the weight of artificial stability.
The resistance training prescribed? A futile gesture against the tide of pharmacological nihilism. We seek to rebuild muscle while the soul atrophies. The real question: Why do we tolerate this? Why do we accept that healing requires more chemicals, more machines, more control?
Perhaps the answer lies not in the gym, but in the quiet. In letting go. In reducing not just the dose of prednisone-but the dose of our desperation.
December 3, 2025 AT 04:33
Daisy L
OMG I’ve been waiting for someone to say this!! I’m 43, on prednisone for vasculitis, and I’ve been too embarrassed to tell anyone I can’t get off the toilet without using my hands. I thought I was just ‘lazy’ or ‘out of shape.’ Turns out I’ve got steroid myopathy-and I’m not alone!!
I started doing chair squats in my living room every morning. Now I can stand up without grabbing the arms. I feel like I’ve reclaimed my body. I’m not ‘fixed’-but I’m not a prisoner anymore. THANK YOU.
December 4, 2025 AT 20:32