St. John’s Wort might seem like a harmless natural fix for low mood, but it’s not the gentle herb many assume it to be. If you’re taking any prescription medication, this supplement could be quietly sabotaging your treatment-sometimes with life-threatening results.
How St. John’s Wort Changes How Your Body Handles Medications
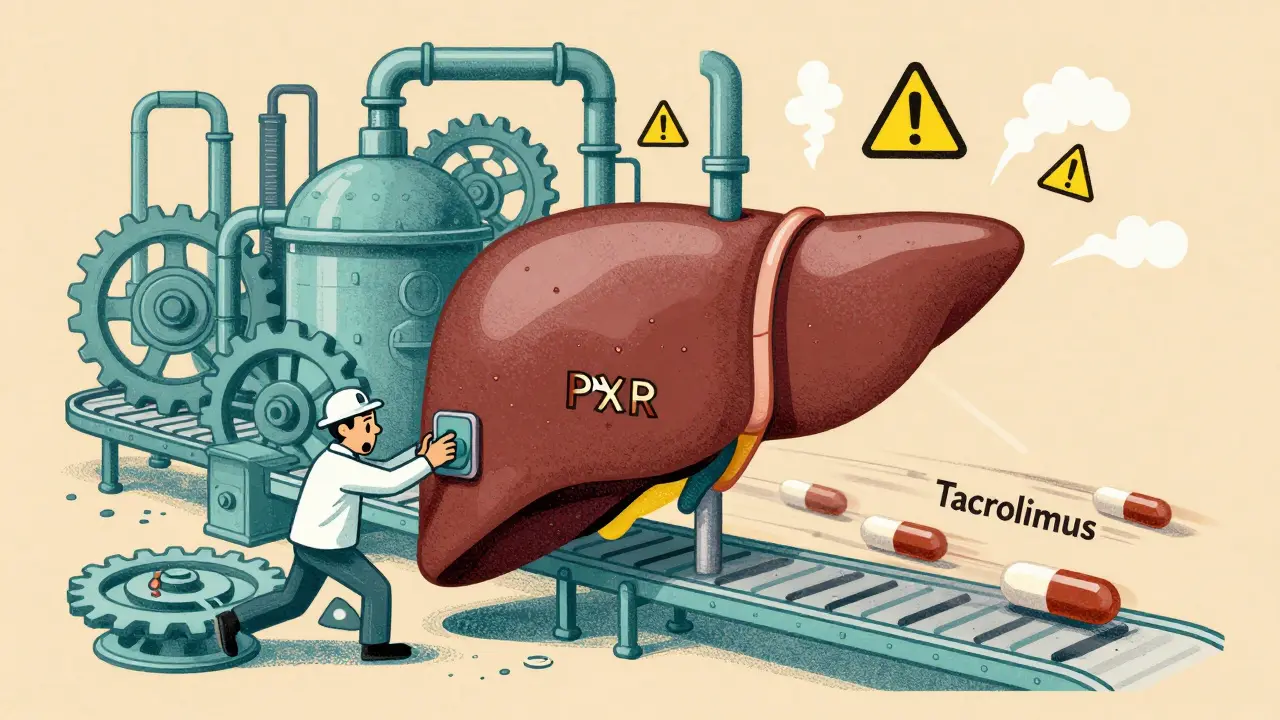
St. John’s Wort doesn’t just sit in your system. It actively rewires how your body processes drugs. Its main active ingredient, hyperforin, turns on a master switch in your liver called the pregnane-X-receptor (PXR). When this switch flips, your body starts producing more of certain enzymes-especially CYP3A4, CYP2C9, and CYP1A2-that break down medications faster than normal.
Think of it like this: your body is a factory that normally takes 8 hours to process a pill. St. John’s Wort tells the factory to double its speed. Now that same pill is gone in 4 hours. The result? The drug never reaches the level it needs to work.
This isn’t theoretical. In 2019, a 34-year-old woman who’d just had a kidney transplant had her tacrolimus levels drop from 12 ng/mL to 3 ng/mL within weeks of starting St. John’s Wort. Her body was rejecting the new organ. She was hospitalized. Her transplant was nearly lost.
Medications That Can Fail Because of St. John’s Wort
There are over 50 known interactions, but some are far more dangerous than others. Here are the ones that can kill you if ignored:
- Immunosuppressants like cyclosporine, tacrolimus, and sirolimus-used after organ transplants. If these drop too low, your body attacks the new organ. Documented cases of organ rejection are not rare.
- HIV medications such as protease inhibitors (ritonavir, indinavir) and non-nucleoside reverse transcriptase inhibitors. These drugs keep the virus under control. St. John’s Wort can make them useless, leading to drug-resistant HIV.
- Anticoagulants like warfarin. One patient’s INR (a measure of blood clotting) dropped from 2.5 to 1.4 in just 10 days after starting St. John’s Wort. That’s the difference between safe blood thinning and a stroke.
- Oral contraceptives. Birth control pills can become ineffective. There are documented cases of unintended pregnancies in women who took St. John’s Wort while on the pill.
- Antidepressants like SSRIs and SNRIs. Mixing them with St. John’s Wort can trigger serotonin syndrome-a rare but deadly condition where your brain gets flooded with serotonin. Symptoms: high fever, seizures, rapid heartbeat, confusion.
- Pain medications like oxycodone, methadone, and tramadol. St. John’s Wort can make these painkillers stop working. Patients report sudden, unexplained pain flare-ups after starting the herb.
The European Medicines Agency says it clearly: don’t use St. John’s Wort with any drug that has a narrow therapeutic index-that means the difference between the right dose and a toxic dose is tiny. These are the drugs you can’t afford to mess with.
Why You Might Not Realize Something’s Wrong
One of the most dangerous things about St. John’s Wort is how slow the effects are. You won’t feel sick right away. The enzyme induction takes about 10 days to peak. And even after you stop taking it, the effects can linger for two weeks.
People often don’t connect the dots. A woman on birth control gets pregnant. She blames herself, not the supplement she started six weeks ago. A transplant patient feels fine, but their lab work shows dropping drug levels. They don’t know to ask about the herbal tea they’ve been drinking daily.
A 2017 study found most patients take 3 to 6 weeks before they realize something’s off. By then, the damage may already be done.

St. John’s Wort vs. Other Herbal Options
Not all herbal mood boosters are created equal. SAM-e and 5-HTP are often suggested as alternatives. But here’s the catch: they don’t touch your liver enzymes like St. John’s Wort does.
SAM-e has fewer than five documented interactions-mostly with MAO inhibitors, which are rarely used today. 5-HTP has minimal known interactions. Neither has been linked to organ rejection or birth control failure.
St. John’s Wort has more interactions than any other herbal supplement on the market. It’s more like a prescription enzyme inducer-think rifampin-than a mild tea. And unlike prescription drugs, there’s no standardization. One bottle might have 2% hyperforin; another might have 5%. You can’t predict how strong the effect will be.
Who’s Most at Risk?
It’s not just people on complex meds. The average user is a woman between 35 and 54. According to the 2017 National Health Interview Survey, 8.2% of women in that group use St. John’s Wort. Many are self-treating mild depression because they don’t want to take antidepressants-or they think herbal means safe.
Older adults are less likely to use it. That’s not because they’re more cautious. It’s because they’re on more medications. Polypharmacy is a natural barrier. If you’re taking five or more prescriptions, you’re more likely to have been warned off it by your pharmacist.
But here’s the problem: even if you’re healthy now, you might need a transplant, start HIV treatment, or get prescribed warfarin next year. St. John’s Wort doesn’t just affect what you’re taking today-it affects what you might need tomorrow.

What Should You Do?
If you’re already taking St. John’s Wort:
- Stop immediately if you’re on any of the high-risk medications listed above.
- Don’t just quit cold turkey if you’ve been using it for depression. Talk to your doctor about tapering or switching to a safer alternative.
- Get your drug levels checked. If you’re on tacrolimus, warfarin, or birth control, ask for a blood test. It’s the only way to know if your meds are still working.
If you’re thinking about starting it:
- Make a full list of every medication and supplement you take-prescription, over-the-counter, vitamins, herbs.
- Take it to a pharmacist. Not your doctor. A pharmacist sees these interactions every day. They can run a free interaction check in seconds.
- Ask: "Is there a safer way to treat my depression?" There are FDA-approved options with better safety profiles.
The Bigger Picture
St. John’s Wort isn’t going away. Global sales hit $587 million in 2022. In Germany, it’s still one of the top 5 treatments for depression. But the tide is turning.
The FDA updated its guidance in March 2023, calling St. John’s Wort a "high-risk supplement." The European Medicines Agency requires warning labels on every product. And researchers are now testing hyperforin-free extracts that might keep the mood benefits without the dangerous enzyme induction.
But until those become widely available, the message is simple: if you’re on any prescription medication, St. John’s Wort is not worth the risk. The consequences aren’t just inconvenient-they’re deadly.
Can I take St. John’s Wort with antidepressants?
No. Combining St. John’s Wort with SSRIs, SNRIs, or MAO inhibitors can cause serotonin syndrome-a dangerous condition that can lead to seizures, high fever, rapid heart rate, and even death. This isn’t a mild side effect. It’s a medical emergency.
How long does St. John’s Wort stay in your system after you stop taking it?
The enzyme-inducing effects can last up to two weeks after you stop taking it. That means even if you quit today, your medications could still be breaking down too fast for the next 14 days. Don’t assume the risk is gone just because you stopped the supplement.
Is St. John’s Wort regulated like a drug?
No. In the U.S., it’s sold as a dietary supplement, so it doesn’t need FDA approval before being sold. The FDA only steps in after problems arise. That’s why labels often lack clear warnings. In Europe, it’s regulated more strictly, with mandatory interaction warnings on packaging.
Can St. John’s Wort affect birth control?
Yes. Multiple cases have been documented where women on birth control pills became pregnant after starting St. John’s Wort. The herb speeds up the breakdown of estrogen and progestin, making the pill ineffective. If you’re on hormonal contraception, avoid it completely.
Are there any safe herbal alternatives to St. John’s Wort for depression?
SAM-e and 5-HTP are two options with far fewer drug interactions. Neither affects liver enzymes the way St. John’s Wort does. But they’re not miracle cures. Their effectiveness is less proven, and they still require medical supervision. Always talk to your doctor before switching.
Why isn’t St. John’s Wort banned if it’s so dangerous?
Because it’s not illegal-it’s a supplement. In the U.S., the FDA can’t ban supplements unless they’re proven to be unsafe in a specific, documented way. St. John’s Wort is legal, but it carries strong warnings in Europe and is flagged as high-risk by the FDA. The burden is on the consumer to know the risks.
What should I do if I’ve been taking St. John’s Wort and I’m about to start a new medication?
Stop taking it at least two weeks before starting the new drug. Tell your doctor and pharmacist you’ve been using it. Ask them to check for interactions. Don’t assume they’ll think to ask. Most doctors don’t routinely ask about herbal supplements unless you bring it up.

Comments
Oluwapelumi Yakubu
Man, I seen this happen in Lagos last year-my cousin was on antiretrovirals and started drinking St. John’s Wort tea because his friend said it ‘cleanses the soul’-next thing you know, his viral load spiked like a rocket. He didn’t even realize the tea was the problem till his doctor pulled up his meds list. Supplements ain’t magic, they’re chemistry-and sometimes, that chemistry is a bomb waiting to go off.
January 5, 2026 AT 03:14
Charlotte N
so i took this for like 3 months last year for anxiety and honestly felt better but i wasnt on anything else… i just… kinda forgot to tell my dr because i thought it was harmless… like tea… but now im scared i might’ve messed something up without knowing…
January 6, 2026 AT 01:55
Jacob Milano
Charlotte, you’re not alone. I did the same thing-thought ‘natural’ meant ‘no consequences.’ Turned out my thyroid med was barely registering. Got a blood test after reading this post and my levels had dropped 40%. I’m not mad at myself, just mad that no one warned me. This stuff needs warning labels bigger than cigarette packs.
January 6, 2026 AT 21:49
Allen Ye
Let’s not romanticize herbalism as some ancient wisdom-it’s just unregulated pharmacology with a yoga mat attached. The PXR activation mechanism isn’t some mystical force; it’s a biological hijacking. Hyperforin doesn’t care if you call it ‘plant medicine’ or ‘spiritual cleansing.’ It binds to nuclear receptors like a corporate raider taking over a company. The FDA’s hands are tied because of the DSHEA loophole, not because the science is unclear. We’ve known this since the 90s. The fact that this is still sold next to gummy vitamins in Walmart is a failure of public health infrastructure, not consumer ignorance. We treat supplements like tea, but they behave like drugs-because they are drugs. The only difference is accountability.
January 8, 2026 AT 18:39
saurabh singh
Bro in India we call this ‘hypericum’ and folks use it like chai-no big deal. But I tell my cousins on blood pressure meds or epilepsy pills: ‘Don’t mix. Your body ain’t a lab experiment.’ One guy got dizzy and passed out after combining it with his antidepressant. Got lucky, no seizures. But still. We need more education, not fear. Maybe community health workers can hand out simple flyers in local languages. No jargon. Just: ‘This herb kills your pills.’
January 8, 2026 AT 23:47
Chris Cantey
Interesting. So the real villain here isn’t the herb-it’s the system that lets it be sold without the same scrutiny as pharmaceuticals. The same people who scream about Big Pharma are the ones drinking this stuff like it’s a blessing. Cognitive dissonance is alive and well in the wellness aisle.
January 10, 2026 AT 06:24
en Max
It is imperative to recognize that the pharmacokinetic modulation induced by hyperforin-mediated upregulation of cytochrome P450 isoforms constitutes a clinically significant, evidence-based risk factor for therapeutic failure in medications with narrow therapeutic indices. The absence of standardized dosing and the lack of mandatory labeling in the U.S. regulatory framework exacerbate this risk. It is strongly recommended that all patients undergoing polypharmacy undergo a comprehensive pharmacovigilance review prior to initiating any herbal supplement, particularly those with documented enzyme-inducing properties.
January 12, 2026 AT 00:46
Terri Gladden
OMG I JUST REALIZED I’VE BEEN TAKING THIS WITH MY BIRTH CONTROL FOR 8 MONTHS… I THINK I’M PREGNANT?? I’M SO SCARED I’M CRYING RIGHT NOW… I JUST THOUGHT IT WAS A ‘NATURAL MOOD BOOSTER’… I’M SO STUPID…
January 13, 2026 AT 15:21
mark etang
Thank you for this critical public health disclosure. The data presented is unequivocal and underscores the urgent necessity for enhanced patient education, pharmacist-led intervention protocols, and regulatory reform regarding botanical dietary supplements. This is not an isolated incident-it is a systemic vulnerability requiring immediate mitigation. I urge all healthcare institutions to implement mandatory screening for herbal supplement use during medication reconciliation.
January 15, 2026 AT 04:54