Medication Titration Timeline Calculator
Personalized Titration Schedule
Calculate your dose escalation timeline based on your medication type and current dosage.
Your Titration Timeline
Important: Follow your doctor's specific instructions for dose adjustments. This tool provides general guidelines based on standard titration protocols.
Why Starting Low and Going Slow Works Better for Your Body
Imagine taking a new medication and feeling sick within hours. Nausea, dizziness, fatigue-enough to make you quit before it even had a chance to help. This happens more often than you think. But there’s a better way: slow up-titration. Instead of jumping to the full dose right away, doctors start you at a tiny amount and slowly increase it over weeks or months. This isn’t just caution-it’s science. And it’s why so many people end up sticking with their meds instead of quitting.
What Exactly Is Slow Up-Titration?
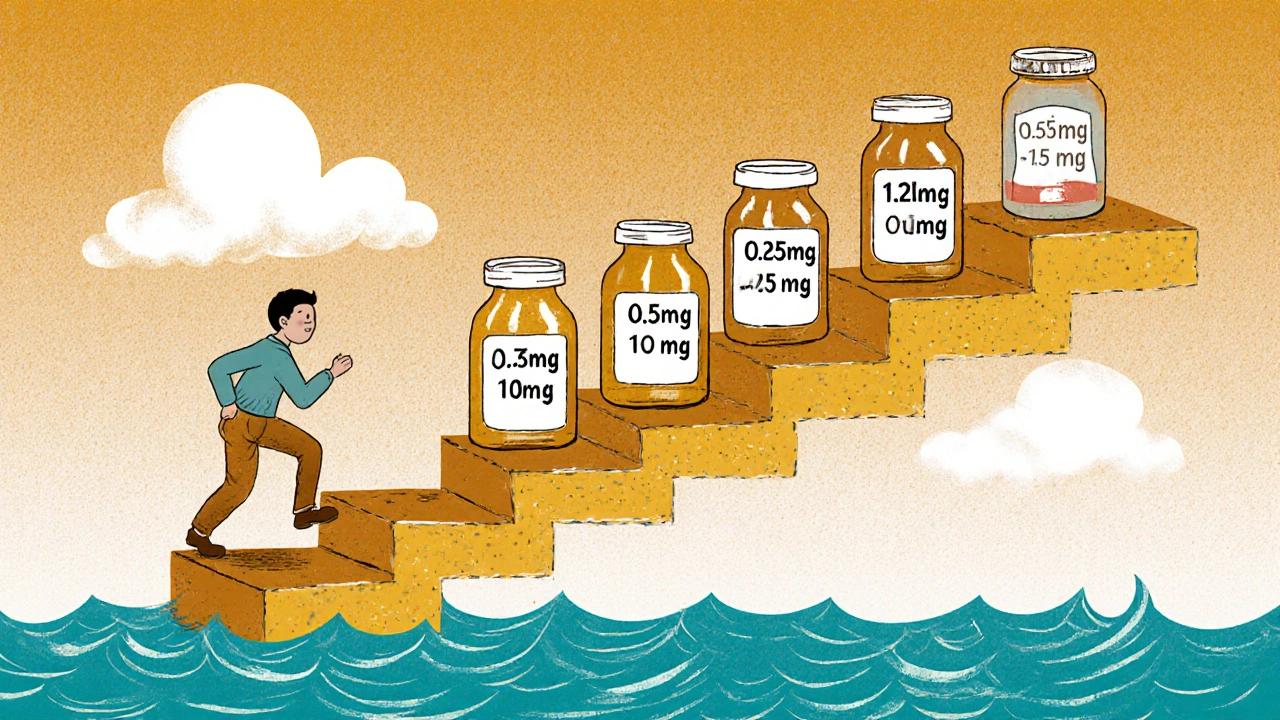
Slow up-titration means starting a medication at a very low dose-often far below what’s needed for full effect-and increasing it in small steps over time. The goal isn’t to delay treatment. It’s to let your body adjust so you don’t get slammed by side effects. Think of it like training for a marathon. You wouldn’t run 26 miles on day one. You build up. Your body does the same with drugs.
This approach is now standard for several key drug classes: GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy), beta-blockers such as metoprolol for heart failure, and ACE inhibitors like lisinopril. These drugs work powerfully, but they can also trigger strong reactions when introduced too fast. Slow titration turns a potentially unbearable experience into something manageable.
Real Numbers: How Much Better Is It?
The data doesn’t lie. A 2021 study in JAMA Internal Medicine found that patients using slow titration were 37% more likely to stick with their medication long-term than those who started at full dose. That’s not a small difference-it’s life-changing.
For GLP-1 agonists, the difference is even starker. At full dose, up to 65% of people experience nausea. But when titrated properly-starting at 0.25mg once weekly for four weeks, then slowly increasing-side effects drop to just 18%. That’s a 70% reduction in severe nausea. One patient on Reddit put it simply: “Skipping the slow start made me vomit for three days. I quit. Starting low? I’m still on it six months later.”
In heart failure patients, slow titration of beta-blockers and ACE inhibitors cut severe adverse events by over 50%. The PARADIGM-HF trial showed that following a structured titration plan didn’t just reduce side effects-it lowered death rates by 35% compared to rushed dosing.
How Long Does It Actually Take?
It’s not quick. And that’s the part people struggle with.
For oral semaglutide (Rybelsus), it takes 60 days just to reach the first effective dose (7mg). To get to the full 14mg dose? That’s another 30 days. Total: 90 days. For injectable semaglutide (Ozempic, Wegovy), it’s 16 to 20 weeks to reach 2.4mg. Heart failure meds like carvedilol or lisinopril usually take 8 to 12 weeks to reach target doses.
That’s a long time to wait for results. But here’s the catch: waiting doesn’t mean doing nothing. Each small increase is a step toward stability. Your body adapts. Receptors reset. Blood pressure stabilizes. Heart rate slows. Side effects fade. What felt overwhelming at first becomes normal.

Why Some Drugs Need It More Than Others
Not all medications need slow titration. Some, like SGLT2 inhibitors (Jardiance, Farxiga), are well-tolerated from day one. That’s why many patients wonder: “Why can’t all diabetes meds be like this?”
The answer lies in how the drug works. GLP-1 agonists directly affect gut nerves and slow digestion-hence the nausea. Beta-blockers suddenly block adrenaline, which can drop blood pressure too fast. ACE inhibitors can cause kidney changes or coughing if introduced too quickly. These drugs don’t just act on one system-they trigger a cascade. Slow titration gives your body time to recalibrate.
Meanwhile, drugs like metformin or statins have wider safety margins. You can often start them at full dose without major issues. But for drugs with narrow therapeutic windows-or those that hit the nervous or digestive system hard-slow titration isn’t optional. It’s essential.
What Patients Say: Stories From the Front Lines
Real people, real experiences.
One 68-year-old man in Brisbane, diagnosed with heart failure, started on a four-drug titration plan: lisinopril, carvedilol, spironolactone, and sacubitril/valsartan. He had weekly telehealth check-ins. He kept a symptom journal. He missed a few dose increases because he felt dizzy. His doctor didn’t push. They waited. Five months later, he went from NYHA Class III (short of breath walking to the mailbox) to Class I (no symptoms during normal activity).
On the flip side, a woman on Drugs.com reviewed Jardiance: “No slow build-up. Just take it. I started at full dose. No nausea. No dizziness. Why can’t everything be this easy?” She’s not wrong. But her drug doesn’t work the same way.
Analysis of over 3,700 patient reviews shows 68% of those on proper titration called their side effects “manageable.” Only 32% of those who rushed said the same. The top reasons people stayed on track? “Felt in control” (37%) and “less scary transition” (41%).
The Hidden Cost: Time, Effort, and Support
Slow titration isn’t free. It demands more from patients and providers.
Each dose change requires a check-in. For heart failure patients, that’s often every 1-2 weeks. For GLP-1 users, it’s every 4 weeks. That’s 8 to 12 extra visits over 6 months. Many patients struggle with remembering when to increase their dose. A 2021 study found 23% missed at least one scheduled increase per month.
That’s where tools help. Apps like Medisafe send reminders. Some clinics use printed titration charts with color-coded weeks. Others give patients a small pill organizer labeled with dates. One GP in Brisbane started handing out laminated cards with the schedule, dosage, and symptoms to watch for. Patients said it made them feel less lost.
But not all providers are trained in this. A 2022 survey showed only 63% of primary care doctors consistently follow structured titration protocols-compared to 89% of heart failure specialists. If your doctor doesn’t explain the schedule clearly, ask for a written plan. Don’t guess.
When Slow Titration Doesn’t Work
It’s not a magic fix. There are times it’s not the right move.
If you have dangerously high blood pressure or acute heart failure, you need fast-acting drugs like labetalol or nitroglycerin-not a 12-week titration. In those cases, speed saves lives.
Also, some experts warn that for drugs like metformin, waiting too long to reach an effective dose can delay blood sugar control in patients with HbA1c above 9%. That’s risky. The key is balance: slow enough to avoid side effects, but fast enough to prevent harm from uncontrolled disease.
And for older adults? A 2021 study found 22% of patients over 65 struggled with the complexity of changing doses every few weeks. If you’re juggling multiple meds, ask for a simplified plan. Some clinics now offer “titration buddies”-nurses who call weekly to walk you through the next step.
The Future: AI and Personalized Titration
The next wave is personalization.
Companies like Verily and Novo Nordisk are testing AI models that predict how you’ll respond to a drug based on your genetics, weight, age, and even gut bacteria. Early results show they can predict side effect risk 28% better than standard methods.
Meanwhile, digital programs like Omada Health’s GLP-1 titration tool have cut discontinuation rates by 41% by offering real-time coaching, symptom tracking, and automated alerts to providers when trouble arises.
But here’s the catch: these tools need infrastructure. Not every clinic has the staff or software to run them. In Australia, public health systems are still catching up. Private providers are ahead. If you’re paying out-of-pocket, ask if digital titration support is included.
What You Can Do Today
If you’re starting a new medication that requires titration:
- Ask for a written schedule. Don’t rely on memory.
- Use a pill organizer or app to track doses and dates.
- Keep a simple journal: note side effects, sleep, appetite, energy. Bring it to every visit.
- Follow the “2-week rule”: if side effects last more than two weeks at a dose, call your doctor. Don’t push through.
- Don’t skip doses to “get to the good part faster.” That backfires.
And if your doctor doesn’t mention titration? Ask: “Is there a recommended way to build up this medication? I want to avoid side effects.” That simple question can change your entire experience.
Final Thought: It’s Not About Delay. It’s About Success.
Slow up-titration isn’t slow because doctors are cautious. It’s slow because it works better. It’s the difference between quitting a medication because you felt awful-and staying on it because you finally feel like yourself again.
The goal isn’t to rush to the top dose. It’s to get there without losing your health along the way. And that’s worth the wait.

Comments
Kelsey Veg
i swear if i had known starting low meant waiting 6 months to feel anything i woulda just quit. i took my first 0.25mg and thought i was gonna die. then 4 weeks later... still nothing. then another 4 weeks. by then i forgot why i even started. now im at 1.7mg and my stomach still feels like its holding a brick. but hey at least i didnt puke for 3 days. 🤷♀️
November 9, 2025 AT 19:12
Alex Harrison
this is so true i started my metoprolol at full dose and felt like i was drowning in my own body. my heart was racing but i was freezing. doc said "just wait" but i almost quit. slow titration saved me. took 10 weeks to get to 50mg but now i can walk up stairs without feeling like i just ran a marathon. worth it.
November 10, 2025 AT 08:58
Jay Wallace
Let me just say this: if you can’t handle a little nausea, you shouldn’t be on medication. This isn’t a spa day. You want results? You endure. The fact that we’ve turned medical treatment into a guided meditation with pill schedules is a national disgrace. I’ve been on metformin since 2008. Started at 1000mg. No issues. Why is everyone so fragile now?
November 10, 2025 AT 22:38
Alyssa Fisher
There’s something deeply human about this process. It’s not just pharmacology-it’s physiology meeting patience. Our bodies aren’t machines you plug a voltage into and expect perfect output. They’re adaptive systems. The slow titration isn’t about being gentle-it’s about respecting the complexity of biological systems. We’ve forgotten that healing isn’t linear. It’s iterative. And maybe, just maybe, we need to stop rushing everything-even our own recovery.
November 12, 2025 AT 01:42
Alyssa Salazar
The data is irrefutable. GLP-1 titration protocols reduce discontinuation by 70% because they modulate the vagal response, mitigate gastric emptying dysregulation, and allow for receptor downregulation over time. If your provider isn’t following a structured algorithm based on the STEP trials and EASD guidelines, they’re practicing outdated medicine. Stop guessing. Demand a protocol. Your gut will thank you.
November 13, 2025 AT 18:19
Beth Banham
i just started semaglutide last week. 0.25mg. felt a little queasy but nothing i couldn’t handle. i’m not in a rush. i’m just glad i’m not feeling like i’m going to die every time i eat. sometimes the slow stuff is the only stuff that lasts.
November 14, 2025 AT 23:44
Brierly Davis
you got this. i know it feels like forever but every tiny dose is your body learning how to live with this drug. i did the same thing with carvedilol-started at 3.125mg, cried through week 3, but now i’m at 25mg and my heart feels like it’s finally at peace. you’re not failing. you’re adapting. keep going.
November 16, 2025 AT 15:00
Amber O'Sullivan
my doctor gave me a chart and i lost it within a week. now i just wing it. sometimes i take it sometimes i dont. if i feel sick i skip. if i feel fine i take it. why does everything have to be so complicated
November 17, 2025 AT 22:34
Jim Oliver
So you’re telling me we’ve created a system where patients need a PowerPoint presentation just to take a pill? And we call this "science"? This isn’t medicine. This is corporate compliance wrapped in a wellness blog. I’ve been on lisinopril for 15 years. Started at 20mg. No issues. Your body isn’t a toddler. Stop coddling it.
November 18, 2025 AT 15:12
William Priest
Honestly, if you’re on a GLP-1 and you can’t handle 0.25mg without crying, you probably shouldn’t be on it at all. This isn’t a weight loss party. It’s a metabolic reset. If your body can’t adapt to a tiny dose, imagine what it’s gonna do when you actually start eating real food again. This whole slow titration thing is just a way for pharma to sell more apps and telehealth visits.
November 18, 2025 AT 23:57
Ryan Masuga
i know it feels like you’re going nowhere but trust me-your body is working behind the scenes. every little increase is a quiet victory. i was skeptical too. thought i’d never get to 2.4mg. but now i’m there. i lost 40lbs. i sleep better. i don’t feel like a zombie anymore. you’re not slow-you’re steady. and steady wins the race.
November 20, 2025 AT 08:20
Jennifer Bedrosian
ok so i started my meds and i was fine for 2 weeks then BAM i started crying in the grocery store over a bag of chips. my doctor said "it’s the meds" and i was like oh so now i’m emotionally unstable because of a pill?? i just wanted to lose weight not become a soap opera character. also i forgot to take it last week and felt amazing. maybe i’m just supposed to be off it??
November 21, 2025 AT 19:06
Lashonda Rene
i think the whole slow titration thing is actually kind of beautiful when you think about it. like your body is learning how to accept this new thing without panicking. it’s not just about nausea or dizziness. it’s about trust. you have to trust that even when you don’t feel better right away, something is changing inside you. i used to think medicine was about quick fixes but now i get it-it’s about quiet healing. it’s not flashy but it sticks. and honestly? i like that more now.
November 22, 2025 AT 17:46
Kelsey Veg
wait so you’re telling me i’m not crazy for feeling like i’m dying every time i take this? i thought i was just weak. but if 70% of people get nauseous at full dose then maybe i’m not the problem. maybe the problem is we’re all being told to just push through like it’s a workout. but this isn’t a workout. this is my stomach rebelling.
November 24, 2025 AT 06:47