Secondary Hypogonadism Myth Checker
Which of the following is TRUE about secondary hypogonadism?
Which statement best describes the myth "Low testosterone equals low sex drive"?
What is the recommended diagnostic approach for secondary hypogonadism?
Your Results
When men hear the term secondary hypogonadism, they often picture a single, simple problem that can be fixed with a quick prescription. The reality is messier, and a lot of the talk around it is riddled with myths. This guide pulls apart the most common misconceptions, explains what truly causes low testosterone, and shows how to get accurate diagnosis and sensible treatment.
What is Secondary Hypogonadism?
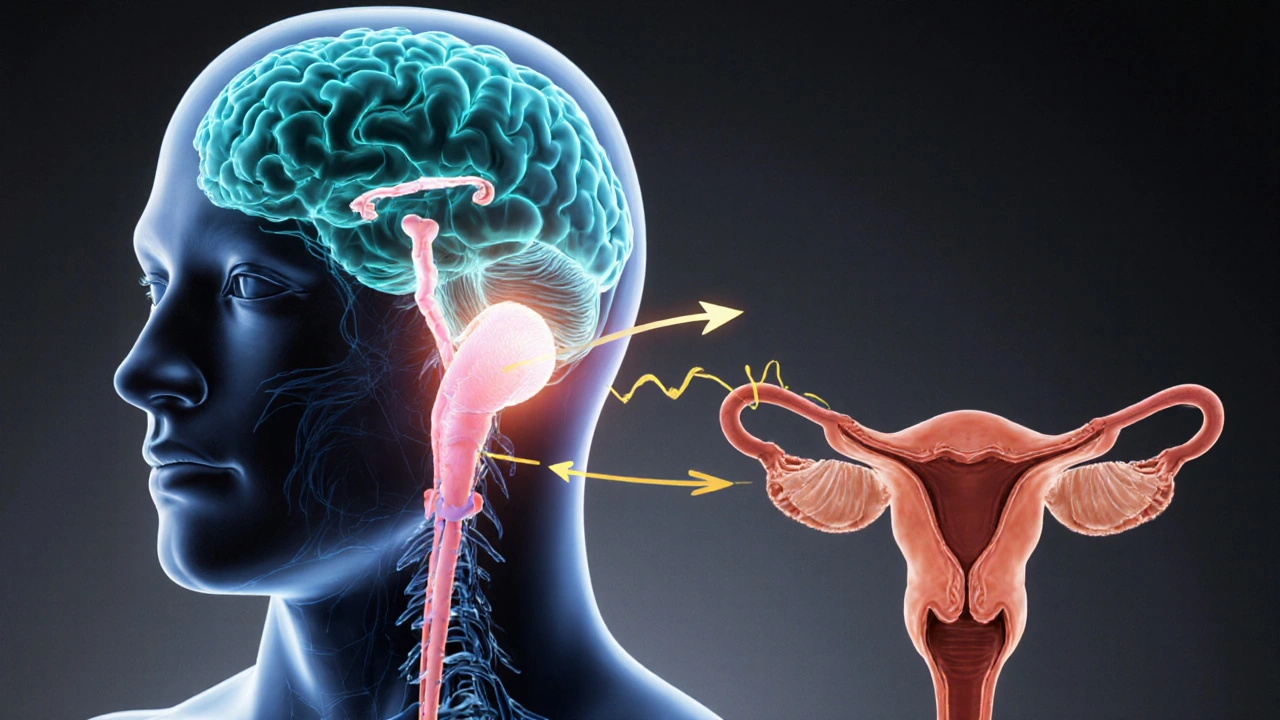
Secondary Hypogonadism is a condition where the testes produce normal amounts of testosterone but the signal to do so is weak or missing. The signal comes from two brain regions: the hypothalamus releases gonadotropin‑releasing hormone (GnRH), prompting the pituitary gland to secrete luteinizing hormone (LH) and follicle‑stimulating hormone (FSH). When this pathway falters, testosterone levels dip even though the testes themselves are healthy.
Myth 1: "It’s Just Getting Older"
Age‑related decline in testosterone, sometimes called “andropause,” is real, but it’s a gradual trend, not a sharp drop that defines secondary hypogonadism. Studies from the Endocrine Society show that men lose about 1‑2% of total testosterone per year after age 30. Secondary hypogonadism, however, often appears suddenly and is linked to specific causes like obesity, chronic illness, or medication side‑effects.
Myth 2: "Low Testosterone Equals Low Sex Drive"
While low libido is a frequent symptom, it’s not exclusive to secondary hypogonadism. Psychological stress, depression, and relationship issues can lower sexual desire even with normal testosterone. Conversely, some men with markedly low testosterone still report a healthy sex drive. The key is to evaluate the full symptom picture - fatigue, reduced muscle mass, anemia, and mood changes - alongside lab values.

Myth 3: "A Single Blood Test Is Enough"
The gold standard for diagnosing secondary hypogonadism involves at least two morning serum testosterone measurements, plus LH and FSH levels. A low total testosterone with inappropriately low or normal LH suggests the problem lies upstream. If LH is elevated, the issue is likely primary hypogonadism. Adding a free testosterone or bioavailable testosterone test can clarify cases where SHBG (sex hormone‑binding globulin) skews total levels.
Myth 4: "All Testosterone Therapy Works the Same"
There are several delivery methods - gels, patches, injections, pellets, and even nasal sprays. Each has a distinct pharmacokinetic profile. For example, intramuscular injections can cause peaks and troughs, leading to mood swings, while daily gels provide steadier levels but carry a risk of skin transfer. Choosing the right format depends on lifestyle, skin sensitivity, and how the body metabolises testosterone.
Myth 5: "Only Men with Very Low Testosterone Need Treatment"
Clinical guidelines from the Endocrine Society recommend treatment when total testosterone falls below 300ng/dL (10.4nmol/L) and symptoms are present. However, some men with borderline levels (300‑350ng/dL) experience significant quality‑of‑life improvements once therapy begins. The decision should be individualized, weighing symptom burden, comorbidities, and patient preference.
Common Triggers of Secondary Hypogonadism
- Obesity - excess fat tissue raises aromatase activity, converting testosterone to estrogen, which suppresses the HPG axis.
- Type 2 Diabetes - insulin resistance interferes with LH secretion.
- Chronic Opioid Use - opioids blunt GnRH release.
- Glucocorticoid Therapy - high-dose steroids suppress hypothalamic signaling.
- Pituitary Tumors - mass effect can impair LH/FSH production.

Myth‑Busting Table
| Myth | Fact |
|---|---|
| Only older men get secondary hypogonadism. | Men as young as 30 can develop it, especially with obesity or chronic disease. |
| Low testosterone always means low libido. | Libido is influenced by many factors; testosterone is just one piece. |
| One blood draw confirms the diagnosis. | Two morning draws plus LH/FSH are required for accurate classification. |
| All testosterone products are interchangeable. | Delivery method affects blood levels, side‑effects, and patient adherence. |
| Treatment is only for men with < 200ng/dL. | Guidelines start therapy at < 300ng/dL when symptoms are present; borderline cases may still benefit. |
How to Navigate Diagnosis and Treatment
- Schedule a morning appointment (7‑9AM) for bloodwork.
- Request a panel that includes total testosterone, free testosterone, LH, FSH, and SHBG.
- Interpret results with a clinician: low testosterone + low/normal LH = secondary hypogonadism.
- Identify and address reversible causes - lose weight, adjust medications, treat sleep apnea.
- If therapy is warranted, discuss formulation options and monitor levels every 3‑6months.
- Track symptoms using a simple diary - energy, mood, libido, muscle strength - to gauge effectiveness.
Potential Pitfalls and How to Avoid Them
- Self‑diagnosing online: Internet symptom checkers can’t replace lab work.
- Skipping follow‑up labs: Testosterone levels can fluctuate; regular monitoring prevents overtreatment.
- Ignoring comorbidities: Treating obesity or diabetes often improves hormone levels without medication.
- Choosing the cheapest product without guidance: Low‑dose gels may not raise levels enough, while high‑dose injections risk polycythemia.
Frequently Asked Questions
Can secondary hypogonadism be cured?
In many cases the underlying cause - such as obesity, medication side‑effects, or pituitary disease - can be treated, leading to restored hormone production. When the root issue isn’t reversible, testosterone therapy manages symptoms.
Is a low LH level always a sign of secondary hypogonadism?
Low or inappropriately normal LH together with low testosterone strongly points to secondary hypogonadism, but acute illnesses and certain medications can transiently suppress LH. Repeat testing is essential.
Should I start testosterone therapy if my level is just under 300ng/dL?
The decision hinges on symptom severity and health background. Many clinicians start therapy at < 300ng/dL when quality‑of‑life is markedly affected, but they also explore lifestyle changes first.
Can exercise boost testosterone without meds?
Resistance training, especially large‑muscle groups, can raise short‑term testosterone spikes and improve body composition, which may modestly lift baseline levels over months.
What are the main side‑effects of testosterone gels?
Skin irritation at the application site is common. Rarely, men experience heightened red blood cell counts (polycythemia) or acne. Proper dosing and regular blood checks keep risks low.

Comments
Gayatri Potdar
They're hiding the real cure behind pharma lies.
October 8, 2025 AT 17:44
Marcella Kennedy
First of all, thank you for sharing such a thorough breakdown of secondary hypogonadism; it’s clear a lot of effort went into demystifying those common myths.
It’s understandable how overwhelming the medical jargon can feel, especially when you’re dealing with symptoms like fatigue, low mood, or changes in libido.
One of the most helpful things is to recognize that low testosterone is rarely an isolated issue-often it’s intertwined with lifestyle factors like weight, sleep, and stress.
When you mentioned the importance of two morning testosterone measurements, that really resonated because many patients rely on a single lab result and get misdiagnosed.
Additionally, the role of LH and FSH as clues to whether the problem is primary or secondary can be a game‑changer for clinicians.
It’s also worth emphasizing that obesity isn’t just a cosmetic concern; excess adipose tissue raises aromatase activity, shifting hormone balance and suppressing the HPG axis.
Similarly, chronic opioid use and high‑dose steroids are notorious culprits that many patients and even some doctors overlook.
In terms of treatment, the variety of testosterone delivery methods-gels, patches, injections, pellets, nasal spray-means there’s likely a formulation that fits any individual’s lifestyle.
But before jumping straight to hormone replacement, I always encourage patients to explore reversible causes first: weight loss, managing sleep apnea, adjusting medications where possible.
Tracking symptoms in a simple diary can provide concrete data to discuss with your endocrinologist and help gauge whether therapy is truly making a difference.
For those who do start testosterone therapy, regular monitoring every three to six months is essential to avoid potential side‑effects like polycythemia or elevated prostate‑specific antigen levels.
And remember, psychological factors such as stress, anxiety, and relationship dynamics play a major role in libido, so addressing mental health alongside hormonal treatment can yield the best outcomes.
In my own practice, I’ve seen men who improved dramatically after modest lifestyle changes, which underscores how interconnected the endocrine system is with overall health.
Lastly, don’t let the “one‑sentence” myths-like “low testosterone always equals low sex drive”-hold you back from seeking a comprehensive evaluation.
Stay curious, stay proactive, and keep advocating for yourself; knowledge truly is the best prescription.
October 12, 2025 AT 00:24
Jamie Hogan
In the grand scheme of endocrinology the discourse surrounding secondary hypogonadism is often reduced to oversimplified soundbites which, frankly, belies the nuanced interplay of hypothalamic signalling and pituitary responsiveness
October 15, 2025 AT 07:04
Ram Dwivedi
Indeed, the hypothalamic‑pituitary‑gonadal axis functions like a delicate orchestra 🎻 each instrument must be in tune for testosterone production to flourish – when the conductor (GnRH) falters, the entire symphony suffers. Understanding this helps us appreciate why merely boosting testosterone downstream may not address the root cause, and why a holistic approach that includes lifestyle, stress management, and neuroendocrine health is paramount.
October 18, 2025 AT 13:44
pooja shukla
Listen, these Western “guidelines” ignore our own population’s genetic makeup and diet – the real solution lies in embracing traditional Indian lifestyle, not foreign hormone gels.
October 21, 2025 AT 20:24
Poonam Mali
Such reductive assertions epitomize the epistemic vacuum perpetuated by anti‑scientific narratives – without rigorous epidemiological data the claim that “Western protocols are irrelevant” collapses under the weight of meta‑analytical evidence supporting individualized endocrine assessment across ethnicities.
October 25, 2025 AT 03:04
Alan Whittaker
What they don’t tell you is that Big Pharma funds the majority of the studies that endorse testosterone gels, ensuring a steady profit stream while keeping the public in the dark about safer natural alternatives.
October 28, 2025 AT 08:44
Michael Waddington
Look, the data is out there – the risk of polycythemia with injectable testosterone is documented, yet the industry downplays it to push pills that are easier to market.
October 31, 2025 AT 15:24
HAMZA JAAN
Some people think a quick quiz can replace a doctor’s insight, but let’s be real – self‑diagnosis on the internet is a recipe for confusion.
November 3, 2025 AT 22:04
April Rios
Philosophically speaking, the pursuit of a singular “cure” mirrors the ancient quest for the elixir of life; in reality, hormone balance is a dynamic equilibrium, not a static endpoint, and acknowledging this complexity is the first step toward genuine understanding.
November 7, 2025 AT 04:44
byron thierry
From a cultural perspective it’s fascinating how different societies frame testosterone discussions – in some regions it’s a taboo, while elsewhere it becomes a badge of masculinity, which inevitably shapes how patients approach treatment options.
November 10, 2025 AT 11:24
bob zika
Indeed, the sociocultural context influences patient expectations; clinicians should therefore incorporate cultural competence into their assessment protocols, ensuring that therapeutic recommendations align with patients’ values and beliefs.
November 13, 2025 AT 18:04
M Black
Hey folks 😃 keep pushing forward – even small lifestyle tweaks like regular strength training and better sleep can boost your natural testosterone levels without the need for meds.
November 17, 2025 AT 00:44
Sidney Wachira
Don’t be fooled by the hype – the “miracle gel” ads are just marketing fluff 😂 the real gains come from consistency in exercise, diet, and stress reduction.
November 20, 2025 AT 07:24
Aditya Satria
Let’s focus on the facts: consistent aerobic activity, adequate vitamin D, and maintaining a healthy weight have all been shown in peer‑reviewed studies to support endogenous testosterone production.
November 23, 2025 AT 14:04
Jocelyn Hansen
Great point! 😊 Remember to set realistic goals and track progress; celebrating even modest improvements can keep motivation high and reinforce positive hormonal changes.
November 26, 2025 AT 20:44
Joanne Myers
In summary, a multifaceted approach that integrates medical assessment with lifestyle modification offers the most robust strategy for managing secondary hypogonadism.
November 30, 2025 AT 03:24
rahul s
All this talk about “global guidelines” forgets that India’s own ancient Ayurvedic principles have long advocated herbal tonics and diet for vigor – why not give them a proper scientific trial?
December 3, 2025 AT 10:04
Julie Sook-Man Chan
I appreciate the thorough overview; it’s a solid foundation for anyone looking to navigate the complexities of secondary hypogonadism.
December 6, 2025 AT 16:44