What Biologic DMARDs Actually Do for Rheumatoid Arthritis
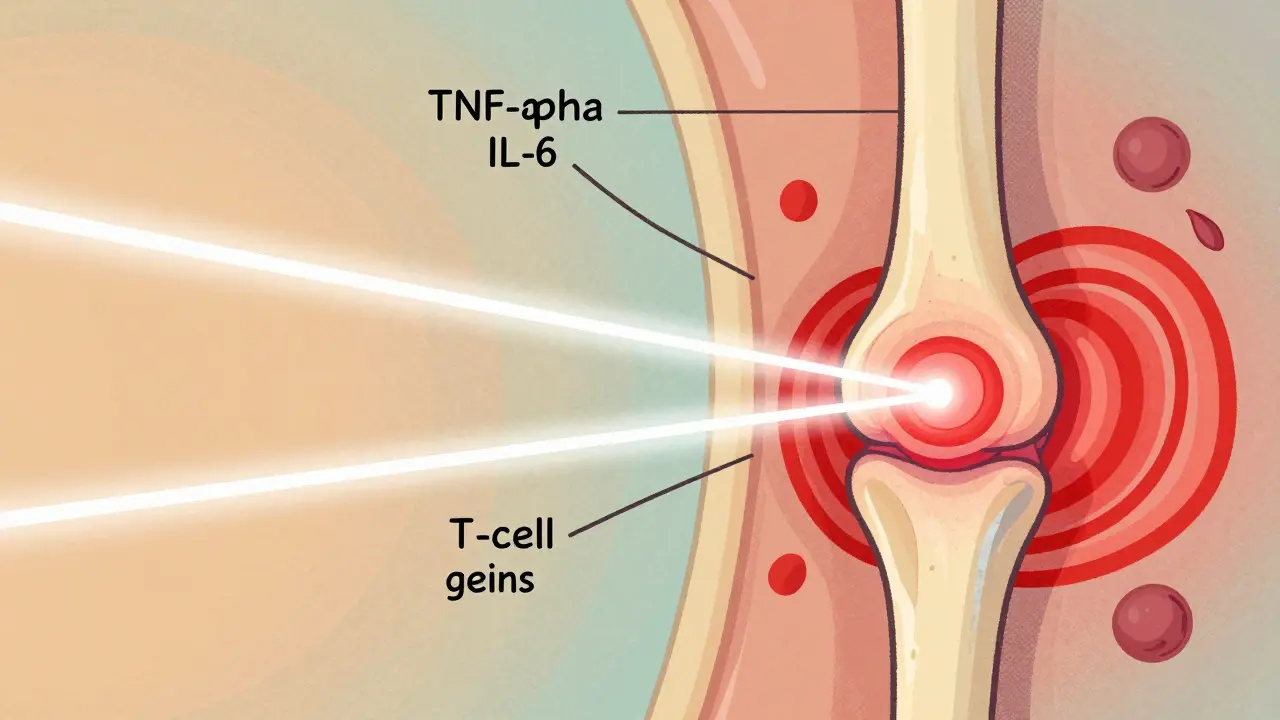
Biologic DMARDs changed everything for people with rheumatoid arthritis (RA). Before they existed, RA was often a slow, relentless march toward joint destruction and disability. Today, for many, it’s a manageable condition - and remission isn’t just a dream. Biologic DMARDs are targeted drugs that shut down specific parts of the immune system driving inflammation in RA. Unlike older drugs like methotrexate, which broadly suppress the immune system, biologics act like precision tools. They block single proteins - like TNF-alpha, IL-6, or T-cell signals - that are overactive in RA. This means less damage to joints, less pain, and a real shot at remission.
The first biologic, etanercept (Enbrel), got FDA approval in 1998. Since then, we’ve seen a wave of new options: adalimumab (Humira), infliximab (Remicade), tocilizumab (Actemra), abatacept (Orencia), and rituximab (Rituxan). Each targets a different piece of the immune puzzle. And while they’re not cures, they’ve turned RA from a life-altering disease into one where many people can live without daily pain or swelling.
Who Gets Biologic DMARDs - And When?
Biologics aren’t the first thing doctors reach for. Methotrexate still is. It’s cheap, well-studied, and works for about half of RA patients. But if you’ve been on methotrexate for 3-6 months and your joints still hurt, swell, or feel stiff - especially if X-rays show early damage - that’s when biologics come into play.
The American College of Rheumatology says biologics are for moderate to severe RA that hasn’t responded to conventional DMARDs. About 30% of RA patients end up needing one. That number rises if you’re younger, have high levels of inflammation markers like CRP or ESR, or show rapid joint damage on scans.
It’s not about how long you’ve had RA - it’s about how active it is. Even someone with five years of RA can still benefit if their disease is still flaring. But if you’ve been in remission for years on methotrexate? You likely don’t need a biologic.
The Big Five Biologic Classes and How They Compare
Not all biologics are the same. They fall into five main groups, each with different strengths and timing:
- TNF inhibitors: Etanercept, adalimumab, infliximab, golimumab. These are the oldest and most used. They often work fast - some people feel better in days. Adalimumab and etanercept are the most effective in real-world studies, beating infliximab by nearly 20% in symptom control.
- IL-6 blockers: Tocilizumab. Slows joint damage and reduces fatigue. Works well for people who don’t respond to TNF blockers. Can be given as a monthly IV or a weekly shot.
- T-cell modulators: Abatacept. Slows down the immune cells that attack joints. Takes longer to work - 3 to 6 months - but lasts long and has fewer infection risks.
- B-cell depleters: Rituximab. Targets B-cells, which make harmful antibodies. Best for people with high levels of rheumatoid factor or anti-CCP antibodies. But if your synovial tissue has few B-cells? It won’t help much.
- JAK inhibitors: Tofacitinib, upadacitinib. These are pills, not shots. They work inside cells, blocking signals that cause inflammation. Upadacitinib beat adalimumab in head-to-head trials, with higher remission rates.
Here’s what the data says about how they stack up:
| Drug Class | Typical Time to Response | Remission Rate (vs. csDMARDs) | Common Administration |
|---|---|---|---|
| TNF inhibitors | 1-4 weeks | 25-40% | Subcutaneous injection (weekly/biweekly) |
| IL-6 inhibitors | 2-8 weeks | 30-45% | IV monthly or SC weekly |
| T-cell modulators | 3-6 months | 20-35% | IV monthly or SC weekly |
| B-cell depleters | 8-12 weeks | 15-30% | IV every 4-8 weeks |
| JAK inhibitors | 2-6 weeks | 35-50% | Oral daily |
One key insight from recent studies: if you don’t respond to one biologic, switching to another in the same class often doesn’t help. But switching to a different type - say, from a TNF blocker to a JAK inhibitor - can work. That’s why matching the drug to your immune profile matters.
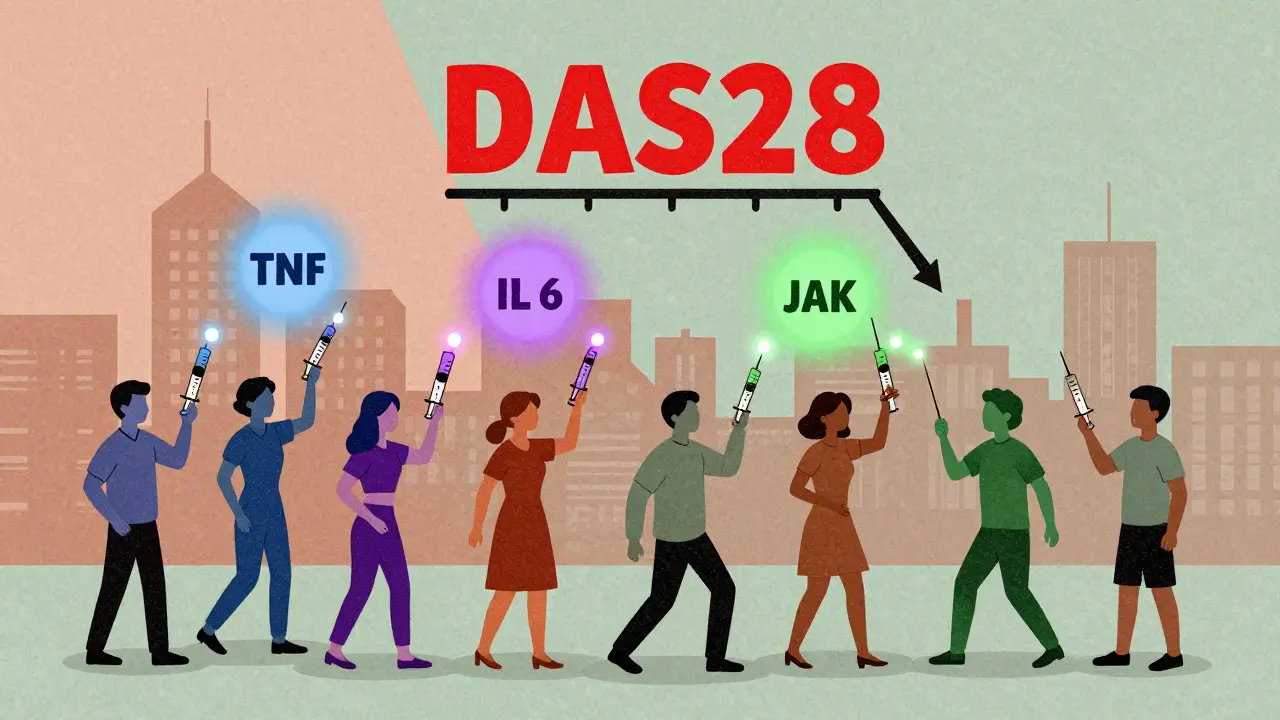
Remission Isn’t Just “Feeling Better” - It’s Measurable
When doctors say “remission,” they don’t mean you’re cured. They mean your disease activity is so low, it’s practically invisible. The DAS28 score - a standard measure based on joint swelling, pain, and blood markers - drops below 2.6. You can move without pain. Morning stiffness lasts less than 15 minutes. Blood tests show normal inflammation levels. And X-rays? No new damage.
With methotrexate alone, only 5-15% of patients reach remission. With biologics? That jumps to 20-50%. In one study, 50% of patients on tocilizumab plus methotrexate were in remission after a year. Another, using upadacitinib, showed 47% remission at 26 weeks.
But here’s the catch: remission doesn’t last forever for everyone. About 40% of people on biologics start losing response after 12-24 months. That’s called secondary non-response. It’s not your fault. It’s biology. Your immune system adapts. That’s why ongoing monitoring is critical. You need regular check-ins with your rheumatologist - not just when you feel bad, but every 3-6 months.
The Real Costs - Money, Side Effects, and Daily Life
Biologics aren’t cheap. In the U.S., they cost $50,000 to $70,000 a year. That’s why many patients turn to biosimilars - cheaper versions of the original drugs. Since 2016, biosimilars have cut costs by 15-30%. In 2023, 35% of TNF inhibitor prescriptions in the U.S. were biosimilars. Many patients report the same results with half the price tag.
Side effects are real. The biggest risk? Infections. Biologics lower your body’s ability to fight off bacteria and viruses. You’re 1.4 times more likely to get a serious infection like pneumonia or tuberculosis. That’s why doctors test for TB before you start. You also need to avoid live vaccines. Flu shots? Fine. Shingles vaccine? Not if you’re on a biologic.
Injection site reactions - redness, itching, swelling - happen in 45% of users. Most fade within days. Fatigue, headaches, and nausea are common too. But here’s what most patients don’t expect: the emotional toll. Some feel anxious about injecting themselves. Others stress over insurance delays. One patient told me, “I cried the first time I gave myself the shot. I didn’t know if I could do it.” But 75% of people master self-injection after just two training sessions.

What Works for One Person Won’t Work for Another
There’s no one-size-fits-all biologic. Your genetics, your immune profile, your joint damage pattern - they all matter. For example:
- If you have high rheumatoid factor and anti-CCP antibodies, rituximab might be your best bet.
- If you’re fatigued and have systemic symptoms like fever or weight loss, tocilizumab often helps more than TNF blockers.
- If you hate needles and want a pill, JAK inhibitors like upadacitinib are a solid option - but they come with a black box warning for blood clots and heart risks in older patients.
Doctors are starting to use synovial tissue biopsies to pick the right drug. In one study, patients with low B-cell signatures responded to tocilizumab 50% of the time - but only 12% responded to rituximab. That’s not random. That’s science guiding treatment.
Dr. Daniel Aletaha from Vienna put it simply: “We’ve moved from trial-and-error to targeted selection. But we’re still learning.”
What Happens After You Start?
Starting a biologic isn’t a one-time event. It’s a lifestyle shift. You’ll need:
- Regular blood tests every 2-3 months to check liver, kidney, and blood cell counts.
- Annual TB and hepatitis screenings.
- Training on how to store your drug (most need refrigeration).
- Understanding how to handle missed doses - don’t double up. Call your rheumatologist.
- A plan for surgery or dental work - you may need to pause your biologic temporarily.
Support systems help. Manufacturer patient programs cover up to 100% of costs for qualifying people. Specialty pharmacies deliver your meds and offer 24/7 nursing lines. Apps like ArthritisPower let you log pain, fatigue, and side effects to share with your doctor.
And yes - many people do get their lives back. One woman from Texas, after 15 years of severe RA, started tocilizumab. Within eight weeks, her DAS28 score dropped from 6.8 to 1.9. She went from using a cane to hiking with her grandchildren. That’s remission. That’s the goal.
The Future: Biosimilars, Longer-Acting Drugs, and Personalized RA Care
The next five years will change how we treat RA even more. Biosimilars will make up 60% of the biologic market by 2027. Longer-acting versions - like a tocilizumab shot you only need twice a year - are in late-stage trials. And research is moving fast toward true personalization.
Scientists are now looking at blood biomarkers and gene patterns to predict who will respond to which drug. Imagine a simple blood test that tells your doctor: “You’ll respond to abatacept, not adalimumab.” That’s not science fiction. It’s happening in labs right now.
Cost will remain a barrier - especially outside the U.S. and Europe. In developing countries, fewer than 10% of RA patients get biologics. That’s not just a medical issue. It’s an equity issue.
But the message is clear: RA doesn’t have to be a life sentence. With the right biologic, at the right time, remission is possible. And for the first time in history, it’s not a miracle. It’s medicine.

Comments
Skye Kooyman
This is the most clear breakdown of biologics I've ever read. No fluff, just facts.
January 27, 2026 AT 06:50
Karen Droege
I've been on tocilizumab for 18 months. My DAS28 was 7.1 when I started. Now it's 1.4. I hiked the Rockies last month with my daughter. This isn't just medicine - it's a second chance. And yes, the IV is a drag, but worth every minute.
January 28, 2026 AT 04:12
Kipper Pickens
The JAK inhibitor data is particularly compelling. Upadacitinib's 47% remission rate at 26 weeks outperforms TNF inhibitors in head-to-head trials. The pharmacokinetic advantage lies in intracellular JAK-STAT modulation, bypassing extracellular cytokine binding inefficiencies inherent in monoclonal antibody platforms.
January 29, 2026 AT 06:33
Dan Nichols
Remission rates are inflated. Most studies exclude patients who drop out due to side effects. You think 50% is good? Try 20% when you factor in real-world non-compliance and infection-related discontinuations.
January 30, 2026 AT 15:48
Renia Pyles
So let me get this straight - you're telling me I have to inject myself with a $70k drug just to avoid using a cane? And if I get pneumonia, it's my fault for being weak? This system is broken.
January 30, 2026 AT 23:55
Neil Thorogood
I gave myself my first Humira shot on a Tuesday. I cried. I threw up. I thought I was dying. Then I did it again. And again. Now I do it while watching Netflix. You're not broken. You're just learning a new skill. 💪
February 1, 2026 AT 01:37
Rakesh Kakkad
In India, these drugs are unaffordable. Even biosimilars cost more than a year's salary for most. We have patients who walk 15 kilometers to clinics because they can't afford the bus fare. This isn't science. It's privilege.
February 2, 2026 AT 20:43
Suresh Kumar Govindan
Biologics are a pharmaceutical scam. They're designed to keep you dependent. The real cure is eliminated inflammation through diet and fasting. Big Pharma doesn't want you to know this.
February 3, 2026 AT 16:09
Faisal Mohamed
The existential weight of chronic illness is often ignored in these clinical narratives. We are not merely immune profiles or DAS28 scores - we are beings navigating the ontological rupture between pre-disease and post-disease selves. The biologic is not a cure; it is a temporary suspension of becoming.
February 5, 2026 AT 11:59
Allie Lehto
i just wanted to say that i read this whole thing and its amazing but like... why do we still have to wait 3 months for abatacept to work?? like can we just fix this already?? #ra #biologics #pleasehelp
February 7, 2026 AT 11:21
Peter Sharplin
I'm a rheumatology nurse. I've seen patients go from wheelchair to walking without pain on these drugs. But I've also seen the fear in their eyes when they hear 'infection risk.' It's not just about the science - it's about trust. Take the time to explain. Listen. They're not just numbers.
February 7, 2026 AT 14:45
Simran Kaur
I’m from Punjab. My mom has RA. She started on a biosimilar last year. She can now hold her grandchild without crying. That’s more than medicine - that’s dignity. Thank you for writing this. It’s the first time I’ve seen our struggle reflected accurately.
February 7, 2026 AT 15:06
eric fert
You know what’s really happening here? The FDA approves these drugs based on trials with 300 people who are all white, middle-class, and have perfect insurance. Then they sell them to everyone else like it’s a one-size-fits-all miracle. Meanwhile, Black and Latino patients are 40% less likely to be prescribed biologics. And you’re all acting like this is progress? It’s not. It’s systemic neglect dressed up as innovation. The real breakthrough? When a poor woman in Mississippi gets the same shot as a CEO in Manhattan. Until then, this is just corporate theater.
February 8, 2026 AT 09:56