When two drugs are supposed to do the same thing, how do you know they actually do? For generic drugs or biosimilars, the old way was simple: give 24 healthy volunteers both versions in a crossover study, take blood every 15 minutes for 48 hours, and compare the average concentrations. But what if the drug is meant for elderly patients with kidney disease? Or babies? Or people on five other medications? That’s where population pharmacokinetics comes in - not as a replacement, but as a smarter tool to prove equivalence when traditional methods fail.
Why traditional bioequivalence studies fall short
Traditional bioequivalence studies rely on tightly controlled conditions: healthy adults, identical dosing schedules, frequent blood draws. They work well for simple oral tablets in healthy people. But they’re useless for drugs used in fragile populations. Imagine trying to test a cancer drug in a 70-year-old with liver failure. Taking 10 blood samples per person isn’t just inconvenient - it’s dangerous. And even if you could, you’d only learn how the drug behaves in a small group that doesn’t represent the real patients who need it. That’s the gap PopPK fills. Instead of forcing people into artificial study conditions, it uses real-world data - the kind collected during routine clinical care. A patient gets their dose, a nurse draws one or two blood samples at random times, and that’s it. Do this across 50 or 100 patients, and you start seeing patterns. Not just averages, but how weight, age, kidney function, or even genetics change how the drug moves through the body.What population pharmacokinetics actually does
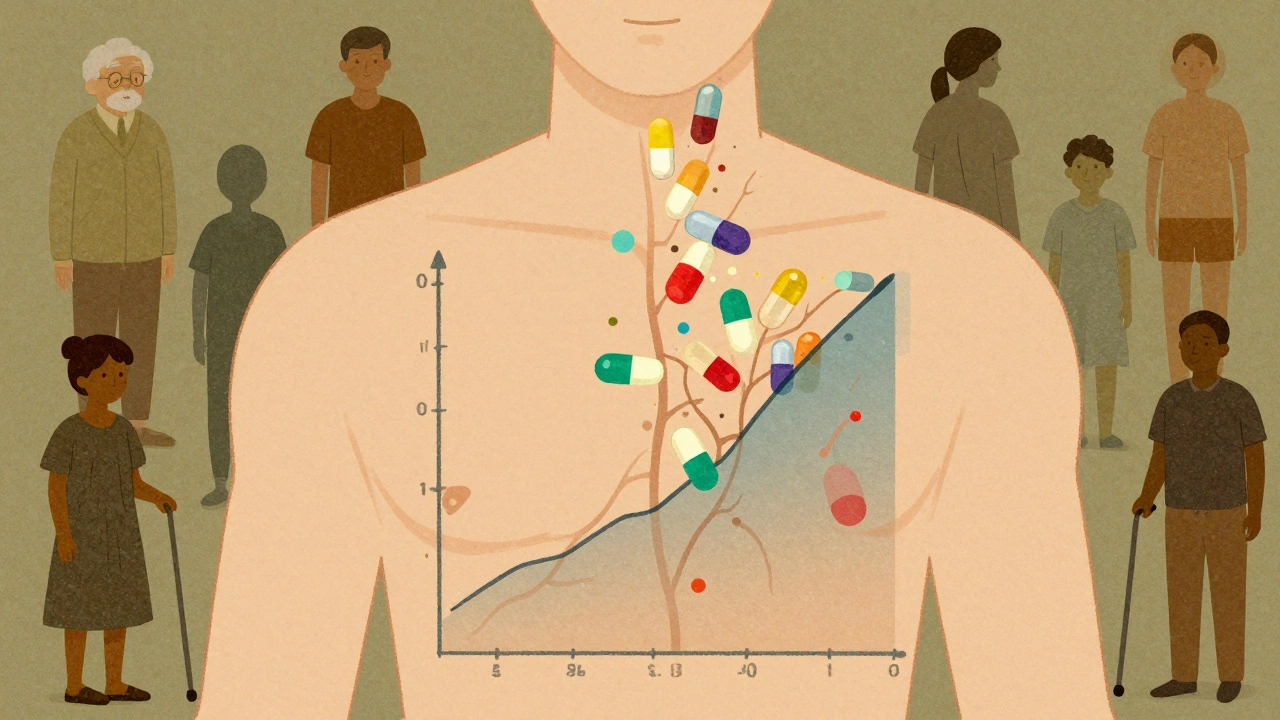
Population pharmacokinetics (PopPK) is a statistical method that looks at drug concentration data from many people at once. It doesn’t assume everyone responds the same. Instead, it asks: What’s the average response? And how much do individuals vary from that average? The core of PopPK is nonlinear mixed-effects modeling. Think of it like this: every person has their own unique drug response curve - shaped by their body size, organ function, or other factors. PopPK finds the overall curve (the population average) and then measures how far each person’s curve deviates from it. These deviations are called between-subject variability (BSV). If BSV is 30%, that means 95% of people will have drug levels within about ±30% of the average. If two formulations have BSVs of 28% and 31%, and both stay within the 80-125% equivalence range, you can say they’re equivalent - even without a traditional crossover study. PopPK also identifies why people differ. Maybe patients with creatinine clearance below 40 mL/min have 40% higher drug exposure. That’s not noise - that’s actionable information. Regulators now expect this level of detail, especially for drugs with narrow therapeutic windows, like warfarin, digoxin, or certain antiepileptics.Regulatory acceptance: FDA and EMA lead the way
The FDA’s 2022 guidance was a turning point. For the first time, they formally said: “Adequate PopPK data can eliminate the need for postmarketing studies.” That’s huge. It means companies can avoid costly, time-consuming trials if they can show through PopPK that their drug performs consistently across key subgroups. The European Medicines Agency (EMA) has been just as supportive since 2014, emphasizing that PopPK can “account for variability in terms of patient characteristics.” Both agencies now accept PopPK for equivalence claims in special populations - neonates, elderly, renal impairment - where traditional studies are unethical or impractical. In fact, between 2017 and 2021, about 70% of new drug applications to the FDA included PopPK analyses. Merck and Pfizer reported that using PopPK reduced the need for extra trials by 25-40% in cases where they successfully demonstrated equivalence across subgroups.
How it’s done: tools, data, and pitfalls
PopPK isn’t done in Excel. It requires specialized software - mostly NONMEM, which has been the industry standard since the 1980s. Monolix and Phoenix NLME are also common. But software alone won’t save you. The biggest challenge isn’t the math - it’s the data. Many clinical trials were never designed with PopPK in mind. Sampling is too sparse, timing is inconsistent, covariates like weight or lab values aren’t recorded. A 2022 survey found 65% of pharmacometricians consider model validation their biggest hurdle. Without high-quality data, even the best model gives misleading results. Another common mistake? Overcomplicating the model. Adding too many covariates - like smoking status, diet, or time of day - without enough data to support them leads to overfitting. The model looks perfect on paper but fails in the real world. The FDA’s analysis of Complete Response Letters from 2019-2021 showed 30% of PopPK submissions needed extra information because of poor model design. Successful PopPK studies start early. Ideally, during Phase 1. That’s when you design the trial to collect the right data - enough samples per person, accurate covariate records, and enough total participants. The FDA recommends at least 40 subjects, but more is better, especially if you’re studying small subgroups.Where PopPK shines - and where it doesn’t
PopPK excels in three areas:- Narrow therapeutic index drugs: Where a 10% change in concentration can cause toxicity or treatment failure.
- Special populations: Kids, elderly, obese patients, those with organ failure - groups excluded from traditional studies.
- Biosimilars: For large molecule drugs, traditional bioequivalence studies are impossible. PopPK is often the only viable path to approval.

The future: machine learning and global standards
The next wave is machine learning. A January 2025 Nature paper showed how AI models can detect hidden, nonlinear relationships between covariates and drug exposure - things traditional PopPK models might miss. For example, maybe a drug’s clearance spikes only when a patient’s sodium level is low and they’re taking a specific diuretic. These complex interactions are hard to model with equations but easy for neural networks to spot. Meanwhile, the IQ Consortium’s Pharmacometrics Leadership Group is working on standardized validation protocols by late 2025. Right now, every company validates models differently. That creates inconsistency. Standardization will make PopPK more reliable and easier for regulators to evaluate. The global pharmacometrics market, fueled by PopPK demand, is projected to grow from $498 million in 2022 to over $1.27 billion by 2029. Nearly all top pharmaceutical companies now have dedicated pharmacometrics teams - up from 65% in 2015 to 92% today.What this means for patients and prescribers
For patients, PopPK means safer, more personalized drugs. Instead of guessing doses based on weight alone, doctors can use models that account for kidney function, age, and other factors to predict exactly how a drug will behave in their body. For prescribers, it means more confidence in generics and biosimilars. You’re not just trusting a label - you’re trusting data that shows the drug performs consistently across the population it’s meant for. And for the system? It means faster approvals, fewer unnecessary trials, and better use of resources. PopPK doesn’t replace traditional bioequivalence - it extends it. Where the old method asks, “Do these drugs behave the same on average?” PopPK asks, “Do they behave the same for everyone?”What is the difference between traditional bioequivalence and population pharmacokinetics?
Traditional bioequivalence studies compare two drug formulations by measuring average drug levels in a small group of healthy volunteers under tightly controlled conditions. Population pharmacokinetics (PopPK) uses real-world data from diverse patient groups to model how drug levels vary across individuals based on factors like age, weight, and kidney function. PopPK doesn’t just ask if drugs are equivalent on average - it asks if they’re equivalent across the whole population.
Can PopPK replace traditional bioequivalence studies entirely?
No, not always. PopPK is best for complex cases - like narrow therapeutic index drugs, special populations (children, elderly, renal impairment), or biosimilars - where traditional studies are unethical or impractical. For simple oral drugs in healthy adults, traditional crossover studies still provide more precise estimates of within-subject variability. Regulators often expect PopPK to complement, not replace, traditional data.
How many patients are needed for a reliable PopPK study?
The FDA recommends at least 40 participants for robust parameter estimation. But the real number depends on the expected variability and the strength of the covariate effects. If you’re studying a small subgroup like neonates, you may need 60-100 patients. More data means better models. Sparsity is a problem - if most patients only have one or two blood samples, you need more total patients to compensate.
Why is model validation such a big challenge in PopPK?
Unlike traditional studies with clear pass/fail criteria, PopPK models are complex and subjective. There’s no single “right” way to build one. Different teams might use different software, covariates, or statistical thresholds. This lack of standardization makes it hard for regulators to compare submissions. A 2022 survey found 65% of pharmacometricians cite model validation as their biggest hurdle. The IQ Consortium is working on standardized validation protocols to fix this.
What software is used for population pharmacokinetics?
NONMEM is the industry standard, used in 85% of FDA-submitted PopPK analyses. Other tools include Monolix, Phoenix NLME, and R packages like mrgsolve. NONMEM dominates because it’s been validated over decades and is accepted by regulators. But it has a steep learning curve - it typically takes 18-24 months of dedicated training to become proficient in both the software and regulatory expectations.
Is PopPK used for biosimilars?
Yes - and it’s often essential. Traditional bioequivalence studies rely on small molecule comparisons, but biosimilars are large proteins with complex structures. You can’t easily measure their concentration the same way. PopPK allows regulators to compare how the biosimilar and reference product behave in the body across diverse patients, making it the primary tool for proving equivalence in this space.
What’s the biggest pitfall in PopPK studies?
Using poor-quality data. Many clinical trials weren’t designed with PopPK in mind, so key covariates (like weight, lab values, concomitant meds) are missing or inconsistently recorded. Another major issue is overparameterization - adding too many variables without enough data, which leads to models that look good on paper but fail in practice. About 30% of PopPK submissions to the FDA required additional information because of these issues.
How does machine learning improve PopPK?
Machine learning helps detect complex, nonlinear relationships between patient factors and drug behavior that traditional models miss. For example, a neural network might find that a drug’s clearance increases only when a patient has low sodium and takes a specific diuretic - a pattern too subtle for standard statistical methods. A 2025 Nature study showed AI-enhanced PopPK models can improve prediction accuracy by up to 20% in some cases.

Comments
Christian Landry
this is wild. i had no idea poppk could replace whole clinical trials. like... we're basically using real patient data to cut costs? 🤯
December 8, 2025 AT 11:51
Stacy Tolbert
i just cried reading this. my mom was on warfarin for 12 years and they kept guessing her dose. if this had been around back then...
December 9, 2025 AT 15:27
Guylaine Lapointe
So let me get this straight: you’re telling me we’re using real-world data from sick people to approve drugs… instead of forcing healthy volunteers to sit in a lab for 48 hours? And you’re calling this progress? This is how we get another Vioxx. I’m not impressed.
December 9, 2025 AT 16:19
Raja Herbal
in india we give 1 pill to 100 people and hope for the best. poppk? sounds like american fancy math to justify skipping real trials.
December 9, 2025 AT 19:46
Katie Harrison
I’ve worked in pharmacometrics for 12 years… and I still get nervous when I see a model with 12 covariates and only 35 patients. It’s not about the math-it’s about whether the data was collected with intention. Too many teams treat PopPK like a magic wand instead of a precision tool.
December 10, 2025 AT 06:51
Ronald Ezamaru
The FDA’s 2022 guidance was a game-changer. I’ve seen companies waste millions running redundant trials because they didn’t design for PopPK from Phase 1. If you’re not collecting covariates-weight, labs, meds-during early trials, you’re just throwing money away. This isn’t optional anymore.
December 11, 2025 AT 01:31
Mona Schmidt
I appreciate how clearly this breaks down the difference between traditional bioequivalence and PopPK. But I’m curious: why do so many submissions still fail validation? Is it lack of training? Poor data collection? Or is it just that regulators haven’t caught up to the science? I’ve seen brilliant models rejected because they used Monolix instead of NONMEM. That’s not science-it’s tradition.
December 11, 2025 AT 06:34
Ryan Brady
So now we’re trusting algorithms over actual human trials? Next they’ll let AI write prescriptions. America’s healthcare is turning into a sci-fi movie and I’m not here for it.
December 11, 2025 AT 17:06
Iris Carmen
popk is cool and all but like... why do we need 40+ people if we're just taking 1-2 blood draws? sounds like a lot of work for not much data. maybe just give the drug and see if people don't die?
December 12, 2025 AT 14:37