More than polypharmacy is just taking too many pills. It’s a silent crisis creeping into the lives of older adults, one prescription at a time. In Australia, nearly 36% of seniors are on five or more medications daily. In nursing homes, that number jumps to over 80%. These aren’t just numbers-they’re real people struggling to keep track of pills, dealing with dizziness from a drug interaction they never knew about, or falling because a medication they’ve been on for years is no longer helping-and maybe even hurting.
What Exactly Is Polypharmacy?
Polypharmacy means taking five or more medications at the same time. It’s not a diagnosis. It’s a consequence. Most older adults aren’t on all those drugs because they want to. They’re on them because they have multiple chronic conditions: high blood pressure, arthritis, diabetes, heart disease, depression, sleep problems. Each condition gets its own prescription. A cardiologist adds one. A rheumatologist adds another. A psychiatrist adds two more. And then there’s the over-the-counter painkiller, the sleep aid, the magnesium supplement, the herbal tea for digestion. No one’s putting it all together. The problem isn’t just the number. It’s the mix. As you get older, your body changes. Your kidneys don’t filter drugs as well. Your liver slows down. Your brain becomes more sensitive to certain chemicals. A dose that was fine at 55 might be dangerous at 75. And when you add five, seven, ten drugs together? The chances of a bad interaction jump from 6% with two drugs to over 50% with five. With seven or more? It’s almost guaranteed something will clash.Why Drug Interactions Are So Dangerous in Older Adults
Think of your body like a complex machine. Each medication is a gear. Too many gears spinning at once? They grind against each other. One drug might make another stronger. Another might cancel it out. Or worse-they might create a side effect that wasn’t there before. Take NSAIDs like ibuprofen. Common for arthritis pain. But when combined with blood pressure meds like ACE inhibitors, they can tank kidney function. Or consider benzodiazepines-used for anxiety or sleep. They cause drowsiness, dizziness, confusion. Add that to a blood thinner like warfarin, and now you’re at higher risk of falling and bleeding internally. One study found that seniors on four or more central nervous system drugs were twice as likely to fall. Then there’s the “prescribing cascade.” A patient starts on a drug. It causes a side effect-say, constipation. The doctor doesn’t stop the original drug. Instead, they prescribe a laxative. Then the laxative causes diarrhea, so they add an anti-diarrheal. Now the patient’s on three drugs for one original problem. And no one’s asking: Do we even need the first one? The most common culprits in older adults? Painkillers (especially NSAIDs), sedatives, anticholinergics (used for overactive bladder, allergies, Parkinson’s), and multiple psychiatric drugs. In fact, nearly half of all visits by seniors on major polypharmacy involve pain medications. That’s not a coincidence. It’s a red flag.Deprescribing: Stopping Meds Is Sometimes the Best Treatment
Deprescribing isn’t about cutting pills randomly. It’s a careful, planned process of reducing or stopping medications when the risks outweigh the benefits. It’s the opposite of adding more. It’s asking: Is this still helping? Is it safe? Could I feel better without it? The American Geriatrics Society’s Beers Criteria and the STOPP/START guidelines are the gold standards here. They list drugs that are risky for older adults-like long-term benzodiazepines, certain antipsychotics for dementia, or multiple antihypertensives when blood pressure is already low. But knowing the guidelines is only half the battle. Using them? That’s where things get messy. Doctors don’t always have time. Patients are scared. “I’ve been taking this for ten years,” they say. “If I stop, what if I get sick again?” Some believe the pill is doing something-even if it’s not. And if a doctor doesn’t bring it up, the patient won’t either. Too often, deprescribing only happens after a bad reaction-like a hospital visit for a fall or kidney failure. But when done right, the results are powerful. In one study, seniors who had a benzodiazepine slowly tapered off saw a 22% drop in falls. Another trial found that reducing unnecessary medications led to fewer ER visits and better quality of life. One woman in her 80s, on eight medications, had chronic dizziness. After reviewing her list, her pharmacist found she was on two drugs that both lowered blood pressure-and neither was actually helping her heart anymore. Once both were stopped, her balance improved. She didn’t need a cane anymore.
Who’s Responsible for Deprescribing?
This isn’t just the doctor’s job. It’s a team effort. Pharmacists are often the first to spot the problem. They see the full list-prescription, OTC, supplements. They know the interactions. But in most clinics, they’re not part of the conversation. In Australia, pharmacist-led medication reviews are growing, especially in community pharmacies and aged care homes. These reviews take 30-60 minutes. They’re not quick checkups. They’re full audits: What’s this for? Is it still needed? Is there a safer alternative? GPs need support too. Many aren’t trained in deprescribing. They’re pressured to meet targets for chronic disease management-check the box, write the script. But managing polypharmacy requires slowing down, not speeding up. Patients and families need education. If you’re caring for an older parent, ask: Why is this medication prescribed? What’s it supposed to do? What happens if we stop it? Bring a list of every pill, capsule, and supplement to every appointment. Write down names, doses, and why they were started.Barriers to Change
Why isn’t deprescribing happening more often? First, the system doesn’t reward it. Doctors get paid for seeing patients and writing prescriptions-not for spending 45 minutes reviewing a medication list. Pharmacist services aren’t always covered by insurance. Medicare doesn’t pay for comprehensive medication reviews unless it’s in a very specific setting. Second, fear. Fear of withdrawal. Fear of symptoms returning. Fear of being seen as negligent. A doctor might hesitate to stop a statin because “it’s been working.” But what if the patient is 90, has no heart disease, and the only side effect is muscle pain that makes walking painful? Is the statin still worth it? Third, fragmentation. A patient sees five different specialists. Each one adds something. No one talks to the others. The GP might not even know what the cardiologist prescribed last month. Electronic health records don’t always talk to each other. Medication lists are outdated or incomplete.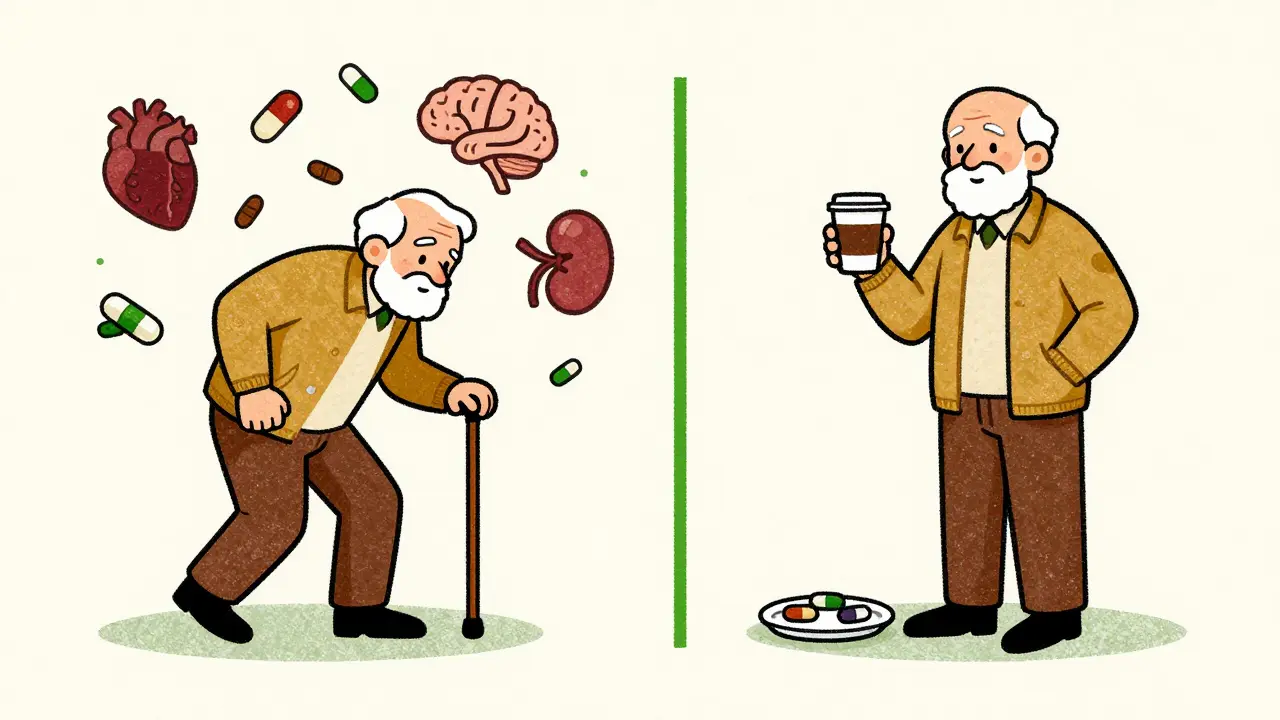
What You Can Do Right Now
If you or someone you care for is on five or more medications, here’s what to do:- Make a complete list of everything: prescriptions, over-the-counter drugs, vitamins, herbal supplements, and even occasional meds like sleep aids or painkillers.
- Bring that list to your next doctor’s appointment. Ask: “Which of these are still necessary?”
- Ask about the goal of each drug. “Is this to prevent something, or to treat symptoms?”
- Ask: “What would happen if we stopped this?”
- Request a pharmacist-led medication review. Many community pharmacies offer this for free or low cost.
- Don’t assume a drug is safe just because it’s been taken for years. Reassess every 6-12 months.
The Future of Medication Safety
New tools are emerging. Some hospitals now use AI to scan medication lists and flag high-risk combinations. Clinical decision support systems in electronic records can warn doctors when they’re about to prescribe something dangerous. But technology alone won’t fix this. People will. The future lies in coordinated care: one team, one plan, one person responsible for the whole picture. It means more pharmacists embedded in primary care. More time in appointments. More training for doctors in geriatric prescribing. More respect for patient goals-like staying independent, avoiding falls, or just feeling well enough to enjoy breakfast with family. The global population of people over 65 will hit 1.5 billion by 2050. If we keep prescribing like we’re trying to fix every symptom with a pill, we’ll drown in hospitalizations, side effects, and preventable decline. But if we learn to step back-to ask not just “what can we add?” but “what can we remove?”-we can give older adults back their safety, their balance, and their peace of mind.What is considered polypharmacy in older adults?
Polypharmacy is generally defined as taking five or more medications at the same time. This includes prescription drugs, over-the-counter medications, supplements, and even occasional or as-needed pills. While the threshold is five, the risk of harm increases significantly with each additional drug, especially when they interact or affect the same body systems.
Are over-the-counter drugs included in polypharmacy?
Yes. Many studies underestimate polypharmacy because they only count prescriptions. But common OTC drugs like ibuprofen, diphenhydramine (Benadryl), or even herbal supplements like St. John’s Wort can cause serious interactions. For example, combining ibuprofen with blood pressure medication can damage kidneys. Benadryl is an anticholinergic and increases fall risk in seniors. Always include everything on your list.
Can stopping medications make you sicker?
Sometimes, but rarely if done properly. Many seniors stop medications out of fear-like stopping a statin because they heard it causes muscle pain. But if the statin isn’t helping (e.g., for someone over 80 with no heart disease), stopping it won’t make them sicker. The real danger is continuing drugs that no longer serve a purpose. Deprescribing is always done gradually and under supervision to avoid withdrawal effects or rebound symptoms.
Who should lead a medication review?
A pharmacist is often the best person to start with. They see the full picture-including prescriptions, OTCs, and supplements-and are trained to spot interactions. But it should be a team effort. Your GP should be involved to approve changes, and specialists should be consulted if a drug was prescribed for a specific condition. In Australia, many community pharmacies offer free medication reviews through the Chronic Disease Management plan.
What are the most dangerous drugs for older adults?
According to the Beers Criteria, high-risk drugs include benzodiazepines (like diazepam), anticholinergics (like oxybutynin for bladder issues), NSAIDs (like ibuprofen), and certain antipsychotics used for dementia. These drugs increase fall risk, confusion, kidney damage, and even dementia progression. Even common drugs like diphenhydramine (found in sleep aids and allergy meds) are on the list because they’re sedating and anticholinergic.
How often should older adults review their medications?
At least once a year, and ideally every six months if on five or more medications. Any time there’s a hospital stay, new diagnosis, or change in health-like a fall or memory issue-review the list immediately. Medications that helped at 70 might not be needed-or could be harmful-at 85.
Is deprescribing safe for people with dementia?
Yes, and often necessary. Many dementia patients are on multiple psychiatric drugs-antipsychotics, antidepressants, sedatives-that can worsen confusion and increase fall risk. Studies show that carefully reducing or stopping these drugs can improve behavior, alertness, and quality of life without worsening dementia symptoms. The key is doing it slowly and monitoring closely.


Comments
Sarah -Jane Vincent
They say polypharmacy is a crisis, but let’s be real-Big Pharma wrote the guidelines. Every pill they push is a profit center. The FDA? Controlled by lobbyists. Your grandma’s ‘necessary’ meds? Half of them were approved because some pharma exec golfed with a senator. And now we’re supposed to trust doctors who get free trips to Hawaii for prescribing statins? Wake up. This isn’t medicine-it’s a corporate scheme disguised as care.
January 14, 2026 AT 20:46
Henry Sy
Man, I’ve seen this shit up close. My pops was on 11 pills-blood pressure, diabetes, sleep, anxiety, pain, probiotics, fish oil, turmeric, vitamin D, melatonin, and some ‘heart tonic’ from the guy at the health fair. One day he started hallucinating. Thought his cat was the president. Turned out it was the damn anticholinergic from his bladder med mixing with the benzo. Doc just added another pill for the ‘side effect.’ Broke my heart. Then his pharmacist said, ‘Let’s kill five of these and see what happens.’ We did. He slept better, walked without a cane, and stopped yelling at the TV. No magic. Just common sense.
January 15, 2026 AT 21:45
Anna Hunger
It is imperative to emphasize that deprescribing must be conducted in accordance with evidence-based clinical guidelines, such as the Beers Criteria and STOPP/START, which have been rigorously validated through peer-reviewed longitudinal studies. Furthermore, the discontinuation of pharmacological agents should be preceded by a comprehensive geriatric assessment, including renal and hepatic function tests, cognitive screening, and medication reconciliation performed by a licensed clinical pharmacist. To proceed otherwise constitutes a breach of the standard of care and may result in iatrogenic harm.
January 17, 2026 AT 00:27
Jason Yan
You know, it’s funny-we treat aging like a disease to be fixed with more pills, but what if it’s just… life? Our bodies slow down, sure, but that doesn’t mean every symptom needs a chemical override. I think we’ve lost something in the last 50 years: the idea that sometimes, less is more. Not just in meds, but in how we live. Maybe if we spent less time chasing perfect biomarkers and more time walking in the sun, eating real food, and talking to people, we wouldn’t need half these drugs in the first place. The system’s broken, but it’s not just about the pills-it’s about what we value. Are we trying to keep people alive, or just keep them from dying in the most expensive way possible?
January 18, 2026 AT 09:05
shiv singh
These doctors are killing our elders with their arrogance. My uncle was 82, healthy as a horse, until they gave him that damn statin. He got muscle pain, then they gave him a muscle relaxer. Then he fell. Then they gave him a blood thinner. Then he bled out in the ER. No one asked if the statin was even needed. He had no heart disease! Just a cholesterol number they were scared of. This is murder by prescription. And the system protects them. Why? Because they’re doctors. Bullshit. They’re just pill pushers with white coats.
January 19, 2026 AT 06:50
Robert Way
i read this and i thought wow this is so true but i also think maybe some of these meds are for real and if you stop them you might die like my aunt took off her blood pressure med and she had a stroke so i dont know maybe its a balance idk
January 19, 2026 AT 15:34
Sarah Triphahn
Let’s be honest-most seniors on polypharmacy are just lazy. They don’t want to change their habits. They’d rather take a pill than eat better or walk more. And their kids? They’re too busy scrolling TikTok to ask questions. It’s not the system’s fault. It’s the people. If you’re 75 and still eating donuts and watching Netflix all day, don’t blame the doctor for giving you a pill to fix the mess you made. Responsibility isn’t dead-it’s just buried under a pile of prescriptions.
January 19, 2026 AT 19:54
Vicky Zhang
I cried reading this. My mom was on 9 meds. She couldn’t remember her own birthday half the time. She’d take the wrong one, then get dizzy, then we’d rush her to the doctor, and they’d just add another one for the dizziness. We finally got a pharmacist to sit down with us for an hour. We cut out three-two sleep aids and that stupid anticholinergic for ‘bladder control.’ She stopped falling. She started laughing again. She remembered my daughter’s name. I swear, it was like she came back to us. No magic cure. Just someone who cared enough to ask, ‘What if we stopped?’ I wish every family had that chance.
January 21, 2026 AT 04:08
Allison Deming
While the sentiment expressed herein is well-intentioned, the article exhibits a dangerous oversimplification of complex geriatric pharmacology. Deprescribing, when performed without individualized risk-benefit analysis, may precipitate rebound hypertension, withdrawal seizures, or uncontrolled psychiatric symptoms. The notion that ‘more pills = bad’ is reductive and ignores the fact that many elderly patients require polypharmacy to survive. To advocate for blanket reduction without longitudinal monitoring is not only irresponsible-it is ethically indefensible. Patient autonomy must be balanced with clinical rigor, not replaced by emotional appeals.
January 23, 2026 AT 00:53
Susie Deer
USA is the only country that lets Big Pharma run the doctors. Other countries don’t have this mess. We need to ban these pills. Take back our health. Stop listening to foreign experts. America knows better. We don’t need no pharmacist reviews. We need strong men and women who don’t take pills. Just get off the couch and live.
January 24, 2026 AT 13:43
TooAfraid ToSay
Wait-so you’re saying the system is rigged? That doctors are just following orders? That this isn’t about health but about control? I’ve been saying this for years. The pills are the new opium. They keep the elderly docile. They don’t want you strong. They want you compliant. And the worst part? You think you’re being cared for. You think you’re safe. But you’re just another number in a spreadsheet. Wake up. This is psychological warfare dressed as medicine.
January 24, 2026 AT 20:52
Dylan Livingston
Oh, how darling. Another feel-good article about ‘deprescribing’ while ignoring the real elephant in the room: we’ve turned aging into a medical problem because we’re terrified of death. We don’t want to sit with our parents as they fade. We want to fix it. So we shove pills down their throats and call it love. But what if the real act of care isn’t adding more drugs-but holding their hand and saying, ‘It’s okay if you don’t get better.’ Maybe the most radical thing we can do is stop trying to fix everything. Maybe healing isn’t in the prescription pad. Maybe it’s in the silence after the last pill is swallowed.
January 26, 2026 AT 03:24
Andrew Freeman
my grandma was on like 7 meds and one day the pharmacist just said ‘stop the benzo and the ibuprofen’ and she was fine. no drama. no hospital. just better. why is this so hard for people to get
January 28, 2026 AT 00:27