Why Opioids for Seniors Need a Different Approach
When a 78-year-old with advanced arthritis can’t walk to the bathroom without agony, opioids might seem like the obvious answer. But giving an older adult the same dose of oxycodone you’d give a 40-year-old? That’s not just risky-it’s dangerous. Seniors don’t process drugs the same way. Their kidneys slow down. Their liver can’t break things down as fast. Body fat increases, water decreases. All of this changes how opioids move through the body-and how long they stay there.
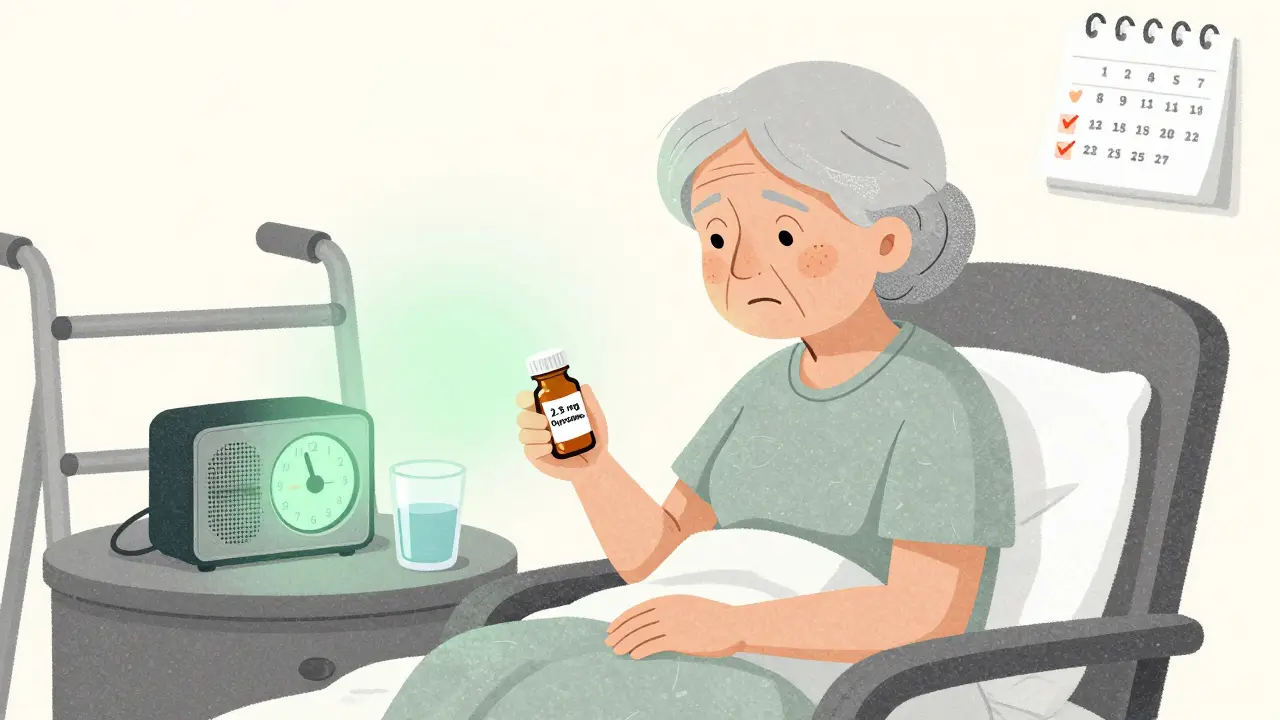
The old rule of thumb-start low and go slow-isn’t just advice. It’s a medical necessity. Studies show that starting at 30% to 50% of the standard adult dose is the safest way to begin opioid therapy for someone over 65 who’s never taken one before. That means if a typical starting dose is 10 mg of oxycodone, a senior might begin with just 2.5 mg or 5 mg. Skipping this step can lead to dizziness, falls, confusion, or even breathing problems that land someone in the hospital.
What Opioids Are Safe for Seniors? Not All Are Created Equal
Not every opioid is suitable for older adults. Some are outright dangerous. Meperidine (Demerol), for example, breaks down into a toxic metabolite that builds up in aging kidneys and can trigger seizures or severe delirium. Codeine is also off-limits because many seniors lack the enzyme needed to turn it into morphine, making it useless-or worse, unpredictable.
Tramadol and tapentadol carry hidden risks too. They affect serotonin levels, and when combined with antidepressants or other medications common in seniors, they can cause serotonin syndrome-a rare but life-threatening condition with high fever, rapid heartbeat, and confusion.
So what’s left? Oxycodone, morphine, hydromorphone, and fentanyl patches can be used, but only with extreme caution. Buprenorphine stands out. It’s a partial opioid agonist, meaning it gives pain relief without the same level of respiratory depression. A 2024 study in the American College of Osteopathic Family Physicians Journal found that low-dose transdermal buprenorphine caused no central nervous system side effects when paired with small doses of oxycodone for breakthrough pain. It also causes less constipation than other opioids, a huge plus for seniors already struggling with bowel issues.
Why Long-Acting Pills and Patches Are a Bad Start
Many doctors reach for long-acting opioids like OxyContin or fentanyl patches because they seem convenient. But for someone who’s never taken opioids before? That’s a recipe for disaster. These formulations release medication slowly over hours. If a senior’s body can’t clear the drug properly, levels build up without warning. The result? Overdose-silent, slow, and often fatal.
Guidelines from the Northwest PA In Guidance (2023) and the Medical Board of California (2022) are clear: never start an opioid-naïve senior on a long-acting form. Always begin with short-acting tablets or liquid. That way, if side effects show up, you can stop the drug quickly. Once the patient has been on a stable dose of immediate-release opioids for several days or weeks, and their response is predictable, then-and only then-can you consider switching to a longer-acting version.

Dosing Limits and What ‘High Dose’ Really Means
The CDC’s 2016 opioid guidelines caused widespread confusion. Clinicians started refusing to prescribe opioids to seniors altogether, fearing they’d hit a 90 MME (morphine milligram equivalent) threshold. But that threshold was never meant for older adults with cancer or end-stage disease. In fact, the CDC itself admitted in 2022 that the 2016 rules were misapplied to these populations.
Today, the focus has shifted from arbitrary numbers to function. Is the patient sleeping? Walking? Eating? That’s what matters. But dose categories still help guide safety:
- Low dose: Up to 40 MME per day
- Medium dose: 41-90 MME per day
- High dose: Over 90 MME per day
For seniors, staying under 40 MME is ideal. Even 50-60 MME can be too much, especially if they’re also on benzodiazepines, sleep aids, or antidepressants. Combining opioids with these drugs multiplies the risk of respiratory depression. A 2023 JAMA Network Open study found that seniors on high-dose opioids plus other sedatives had nearly triple the risk of overdose compared to those on low doses alone.
What to Avoid: NSAIDs, Gabapentinoids, and the Hidden Dangers
Many doctors turn to NSAIDs like ibuprofen or naproxen for seniors with joint pain. But these drugs aren’t safer for older adults-they’re riskier. Long-term use increases the chance of stomach bleeding, kidney failure, and heart attacks. The Northwest PA In Guidance recommends NSAIDs only for short bursts-no more than one or two weeks during flare-ups.
Gabapentin and pregabalin are also commonly prescribed as alternatives. But they don’t work well for most seniors. The same JAMA study showed gabapentinoids reduced pain by less than one point on a 10-point scale-barely better than a placebo. Worse, they cause dizziness, confusion, and falls. In one nursing home study, nearly 1 in 4 seniors on gabapentin fell within three months.
And then there’s acetaminophen. It’s often combined with opioids in medications like Percocet. But seniors can’t handle more than 3 grams per day-and only 2 grams if they’re frail, over 80, or drink alcohol regularly. Liver damage from acetaminophen overdose is silent, sudden, and deadly.
Monitoring Isn’t Optional-It’s Lifesaving
Starting opioids is just the beginning. The real work comes after. The Medical Board of California requires regular check-ins to answer four key questions:
- Is pain improving? (Not just less, but enough to do daily tasks)
- Are side effects manageable? (Constipation, drowsiness, nausea)
- Is cognitive function stable? (Any new confusion or memory lapses?)
- Is there any sign of misuse? (Taking extra doses, running out early, hiding pills)
Monitoring should happen every 1-2 weeks at first, then monthly. Blood pressure, breathing rate, and mental status checks are non-negotiable. Urine drug screens help confirm the patient is taking what’s prescribed and nothing else.
Constipation is almost guaranteed. Don’t wait for it to become a crisis. Start a stool softener like docusate and a stimulant laxative like senna from day one. Hydration and gentle movement help too. If a senior hasn’t had a bowel movement in three days, that’s a red flag.

Functional Goals: The Real Measure of Success
Success isn’t measured by pain scores alone. It’s measured by what the patient can do. Can they get out of bed without help? Can they eat without nausea? Can they sit with family without being too drowsy to talk?
The CDC’s 2022 update pushed this idea hard: treatment goals must be set with the patient, not for them. That means asking: “What’s one thing you want to be able to do that you can’t right now?” Maybe it’s walking to the mailbox. Maybe it’s playing with a grandchild. That becomes the target.
If after four weeks, the patient isn’t closer to that goal-even if their pain score dropped from 8 to 5-then the plan needs to change. Maybe the dose is too high. Maybe the opioid isn’t the right fit. Maybe non-drug options like physical therapy, heat wraps, or cognitive behavioral therapy for pain need to be added.
The Bigger Picture: Opioids Are Just One Tool
Opioids aren’t the first line of defense-they’re the last resort after everything else has been tried. Non-opioid options like topical lidocaine for joint pain, nerve blocks for sciatica, or transcutaneous electrical nerve stimulation (TENS) units can be just as effective with far less risk.
Physical therapy isn’t just for rehab. For seniors with chronic pain, gentle movement programs can improve strength, balance, and pain tolerance over time. Cognitive behavioral therapy helps reframe how the brain processes pain signals, reducing the emotional burden that makes pain feel worse.
And don’t forget the power of simple things: a warm bath, a supportive chair, a daily walk outside. These aren’t “alternative” treatments-they’re foundational.
When to Stop Opioids
There’s no rule that says once you start opioids, you’re stuck forever. If pain improves with other therapies, if side effects become unmanageable, or if functional goals are met, tapering off is not only safe-it’s smart.
Never stop suddenly. Taper slowly: reduce the dose by 10% to 20% every 1-2 weeks. Watch for withdrawal signs: anxiety, sweating, diarrhea, insomnia. If they appear, slow the taper. The goal isn’t to eliminate all pain-it’s to eliminate suffering while keeping the person safe and functional.
Are opioids ever the right choice for seniors with cancer pain?
Yes-opioids remain the first-line treatment for moderate to severe cancer pain in seniors. Studies show a 75% response rate, with an average 50% reduction in pain intensity. The 2022 CDC guideline corrected earlier mistakes by clarifying that rigid dose limits should never apply to patients with cancer, palliative care, or end-of-life needs. The goal is comfort and dignity, not arbitrary thresholds.
Can seniors safely take opioids with other medications?
It depends. Combining opioids with benzodiazepines, sleep aids, antidepressants, or antipsychotics greatly increases the risk of dangerous sedation and breathing problems. Always review all medications with a pharmacist or geriatric specialist. Even over-the-counter sleep aids like diphenhydramine can interact badly. Never assume a medication is safe just because it’s not a prescription.
Why is buprenorphine considered safer for seniors?
Buprenorphine is a partial opioid agonist, meaning it has a ceiling effect-it doesn’t cause the same level of respiratory depression as full agonists like oxycodone or morphine. It also causes less constipation and has a lower risk of delirium. Studies show it can be safely combined with low-dose short-acting opioids for breakthrough pain without causing withdrawal or overdose.
What should I do if my elderly parent is on opioids but seems confused or unsteady?
Contact their doctor immediately. Confusion, dizziness, and unsteadiness are signs of opioid toxicity in seniors. These symptoms can be mistaken for dementia or aging, but they’re often reversible. The dose may be too high, or there could be a dangerous interaction with another medication. Do not wait to see if it gets better-this is an urgent issue.
Is it true that opioids cause addiction in seniors?
True addiction-compulsive use despite harm-is rare in seniors using opioids for legitimate pain. What’s more common is physical dependence, which is normal and not the same as addiction. Seniors on long-term opioids may need to taper slowly to avoid withdrawal, but that doesn’t mean they’re addicted. The real risk is undertreatment of pain, which leads to isolation, depression, and decline.

Comments
owori patrick
Really glad someone laid this out so clearly. I’ve seen too many older folks get prescribed oxycodone like it’s aspirin, then end up falling or confused. Starting at 2.5 mg? That’s the move. My uncle was on 10 mg and couldn’t stand without help-cut it in half, and he was back to watering his plants. No drama, no hospital trips. Just quiet, safe relief.
Also, buprenorphine patches? Absolute game-changer. Less constipation means less suffering overall. And no, you don’t need to be scared of using them even if they’re on other meds-just monitor like you mean it.
January 30, 2026 AT 11:31
Claire Wiltshire
This is one of the most thoughtful, clinically grounded pieces on senior opioid use I’ve read in years. The emphasis on functional outcomes over pain scores is exactly what geriatric care needs.
For example, the point about avoiding long-acting formulations as first-line therapy is not just best practice-it’s lifesaving. I’ve reviewed charts where seniors were started on fentanyl patches after a hip fracture, with no titration period. The results were tragic.
Also, thank you for highlighting the 2022 CDC clarification regarding cancer and palliative care. Too many clinicians still treat all seniors as if they’re at risk for opioid misuse, when the real risk is undertreated pain. Dignity matters.
January 31, 2026 AT 19:05
Darren Gormley
LMAO 😂 so now we’re treating 78-year-olds like fragile glass figurines? ‘Start at 30% of the dose’? Bro. My grandpa took 20mg oxycodone after back surgery at 82 and still drove to church. He didn’t die-he lived. Stop coddling people.
Also, gabapentin doesn’t work? Says who? My aunt’s been on it for 5 years and says it’s ‘magic.’ You’re just scared of real pain management. 😏
February 1, 2026 AT 05:56
Mike Rose
why do docs always overcomplicate stuff? just give the painkiller, done. old people get pain, they need pills. stop with all this MME nonsense and ‘functional goals.’ i just want my grandma to stop screaming. why’s it so hard?
also, buprenorphine? sounds like a drug from star trek. just give her vicodin. problem solved. 🤷♂️
February 2, 2026 AT 22:13
Sheila Garfield
I love how this breaks down what actually matters-function over numbers. My mom’s 84 and was on gabapentin for years. She was always wobbly, didn’t eat well, just sat there. Switched her to low-dose oxycodone + stool softeners? She started cooking again. Took walks. Talked to the neighbors.
And yes, constipation is the silent villain. We started senna on day one, and it made all the difference. No one talks about that enough.
Also, TENS units? Totally underrated. Got one for her knees-she says it’s like a warm hug. Not magic, but real help.
February 3, 2026 AT 10:09
Shawn Peck
STOP. RIGHT. NOW. You’re telling me we can’t give seniors enough pain relief because you’re scared they’ll ‘get confused’? That’s not medicine-that’s punishment. My dad had bone cancer. He was in agony. You want him to ‘walk to the mailbox’? He couldn’t even lift his arm. Opioids saved his last months. Don’t you dare guilt-trip families into letting loved ones suffer because you’re scared of liability.
And buprenorphine? Sure, if you want to play it safe. But if your loved one’s dying? Give them the damn morphine. Let them be comfortable. That’s what matters.
February 4, 2026 AT 08:36
Niamh Trihy
One thing I’d add: urine drug screens aren’t just for catching misuse-they’re for catching *unintended* interactions. I had a patient on tramadol and sertraline who ended up in the ER with serotonin syndrome. No one asked about OTC meds. She was taking NyQuil every night. That’s not addiction. That’s a system failure.
Always ask: ‘What else are you taking?’ Even the ‘harmless’ stuff. And don’t assume seniors know what’s dangerous. Many think ‘natural’ means safe.
February 5, 2026 AT 23:05
Jason Xin
Wow. This post is basically a masterclass. I’m a nurse in a geriatric unit, and I’ve seen the damage from rushed opioid starts. One guy got a 10mg oxycodone tablet because ‘he looked like he needed it.’ He was in a coma for 36 hours.
But honestly? The most important part is the ‘what to avoid’ section. NSAIDs are the silent killers. I’ve lost count of the seniors I’ve seen with GI bleeds from naproxen. And gabapentin? It’s the new valium-overprescribed, under-evaluated.
Also, the constipation point? YES. We start senna and docusate on day one. No exceptions. It’s not optional-it’s basic care.
February 6, 2026 AT 03:30
KATHRYN JOHNSON
This is why America’s healthcare is broken. You treat seniors like children. ‘Start low, go slow.’ ‘Functional goals.’ ‘Avoid NSAIDs.’ Who are you to decide what pain relief a senior deserves? In my country, we give painkillers when needed-no bureaucracy, no fear. If your grandma hurts, you give her the pill. Period.
Stop overthinking. Stop overregulating. Stop treating the elderly like liabilities. They deserve relief, not a risk assessment.
February 6, 2026 AT 09:28