Liver Damage Symptom Checker
This tool helps you identify potential signs of medication-related liver damage. If you're taking any prescription or over-the-counter medications, supplements, or herbal products and experience any of these symptoms, this tool can help you assess your risk.
Remember: Do not use this tool to replace professional medical advice. If you experience jaundice or have two or more of the symptoms listed, seek immediate medical attention.
Symptoms to Check
Select all symptoms you're experiencing that could indicate medication-related liver damage:
Select symptoms to see your assessment
Every year, thousands of people in the UK and across the world develop liver damage from medicines they took exactly as prescribed. It’s not rare. It’s not unusual. And too often, it’s missed until it’s too late. Medication-related liver damage - known as drug-induced liver injury or DILI - doesn’t always come with a warning label. You might be taking a common antibiotic, a painkiller, or even a "natural" supplement, and your liver could be quietly screaming for help.
What Does Liver Damage from Medication Actually Look Like?
Your liver doesn’t complain with a stomach ache. It doesn’t give you a fever right away. Instead, it sends subtle signals that most people dismiss as stress, flu, or just getting older. The first sign? Fatigue that won’t go away. Not just tired - exhausted after a full night’s sleep. Then comes nausea. Not the kind from bad sushi, but a constant, dull feeling in your gut that doesn’t improve with antacids.
But the real red flags show up later. Yellow eyes or skin - jaundice - means your liver can’t process bilirubin anymore. Dark urine, like cola, is another sign. Pale stools? That’s bile not reaching your intestines. And itching - intense, all-over itching without a rash - is one of the most overlooked symptoms. It’s not allergies. It’s your liver failing to clear toxins from your blood.
These signs don’t appear overnight. For most drugs, it takes weeks. Antibiotics like amoxicillin-clavulanate? Often 10 to 20 days after starting. Anticonvulsants? Up to six weeks. Herbal supplements? They can take months. That’s why people think, "It’s not the medicine - I’ve been taking it for weeks." But that’s exactly when damage builds up.
Which Medications Are Most Likely to Hurt Your Liver?
It’s not just the "strong" drugs. Some of the most common prescriptions and supplements carry hidden risks.
- Antibiotics - Amoxicillin-clavulanate (Augmentin) is the top offender, causing liver injury in 1 in 10,000 users. It’s not rare - it’s common enough that doctors should suspect it before ordering a scan.
- Acetaminophen - Yes, Tylenol. More than 50% of acute liver failures in the US are from accidental overdose. The safe limit? 3,000 mg per day for healthy adults. But if you drink alcohol, have liver disease, or take other meds, that drops to 2,000 mg. Many people don’t know that cold medicines, sleep aids, and migraine pills also contain acetaminophen.
- Anticonvulsants - Drugs like valproate and carbamazepine can cause slow, silent damage. People on these for epilepsy or mood disorders often don’t realize their liver enzymes are climbing until they’re hospitalized.
- Herbal supplements - Green tea extract, kava, and turmeric are marketed as "healthy," but they’re now responsible for 20% of DILI cases in the UK. One study found green tea extract caused liver failure in otherwise healthy young adults who took just 2-3 capsules a day for a few weeks.
- Statins - While most people tolerate them fine, a small percentage develop severe liver injury. The European guidelines say it’s extremely rare - under 0.01%. But in the US, the FDA still warns about it. If you’re on a statin and feel unusually tired, get tested.
Here’s the thing: no single blood test confirms DILI. It’s a diagnosis of exclusion. That means your doctor has to rule out viral hepatitis, alcohol damage, autoimmune disease, and gallstones first. That’s why it takes, on average, 28 days to get the right diagnosis - and why 68% of patients are initially misdiagnosed.
When to Act - The 3 Signs That Demand Immediate Care
You don’t need to wait for your next appointment. If you’ve started a new medication in the last 8 weeks and have jaundice plus any two of these, go to the emergency room:
- Dark urine
- Pain in the upper right side of your abdomen (under your ribs)
- Nausea or vomiting that won’t stop
For acetaminophen overdose, time is everything. N-acetylcysteine - the antidote - works best if given within 8 hours of ingestion. After that, every hour reduces its effectiveness by 10%. If you took too many pills, even accidentally, don’t wait. Don’t call your GP. Go to A&E.
And don’t assume "natural" means safe. A 2024 Reddit analysis of 385 cases showed that 29% of DILI cases involved herbal or dietary supplements. One woman in Oxford took 3 turmeric capsules daily for joint pain. Three months later, her liver enzymes were 15 times higher than normal. Her naturopath told her it was "detoxing." It wasn’t. It was failure.
What Happens If You Wait Too Long?
Most cases of DILI reverse once the drug is stopped - if caught early. But if it’s missed, it can lead to acute liver failure. In the US, DILI is now the leading cause of acute liver failure, surpassing hepatitis A and B. About 13% of all acute liver failure cases come from medications.
Those who survive often need a transplant. Those who don’t - well, it’s sudden. No warning. One day you’re tired. The next, you’re in ICU. The average hospital stay for DILI is over 5 days. The cost? Around £15,000 per admission.
And here’s the worst part: nearly 70% of severe cases are preventable. With better awareness, better monitoring, and better communication between patients and doctors, most of these injuries never happen.

How to Protect Yourself - Simple Steps That Save Lives
You don’t need to stop all medications. But you do need to be smarter about them.
- Keep a full medication log - Include every pill, capsule, tea, and supplement. Bring it to every doctor visit. Even the ones you think are "harmless."
- Never exceed acetaminophen limits - 3,000 mg max per day. If you’re over 65, have liver disease, or drink alcohol, stick to 2,000 mg.
- Avoid alcohol with liver-toxic drugs - Alcohol triples or quadruples your risk of damage. That includes wine, beer, cider - anything with alcohol.
- Get liver tests if you’re on high-risk drugs - If you’re taking isoniazid for TB, valproate for seizures, or amoxicillin-clavulanate for a stubborn infection, ask your doctor about a baseline liver test and a follow-up in 2-3 weeks.
- Be skeptical of "detox" supplements - If someone tells you itching or fatigue is "normal" while taking supplements, walk away. It’s not detoxing. It’s damage.
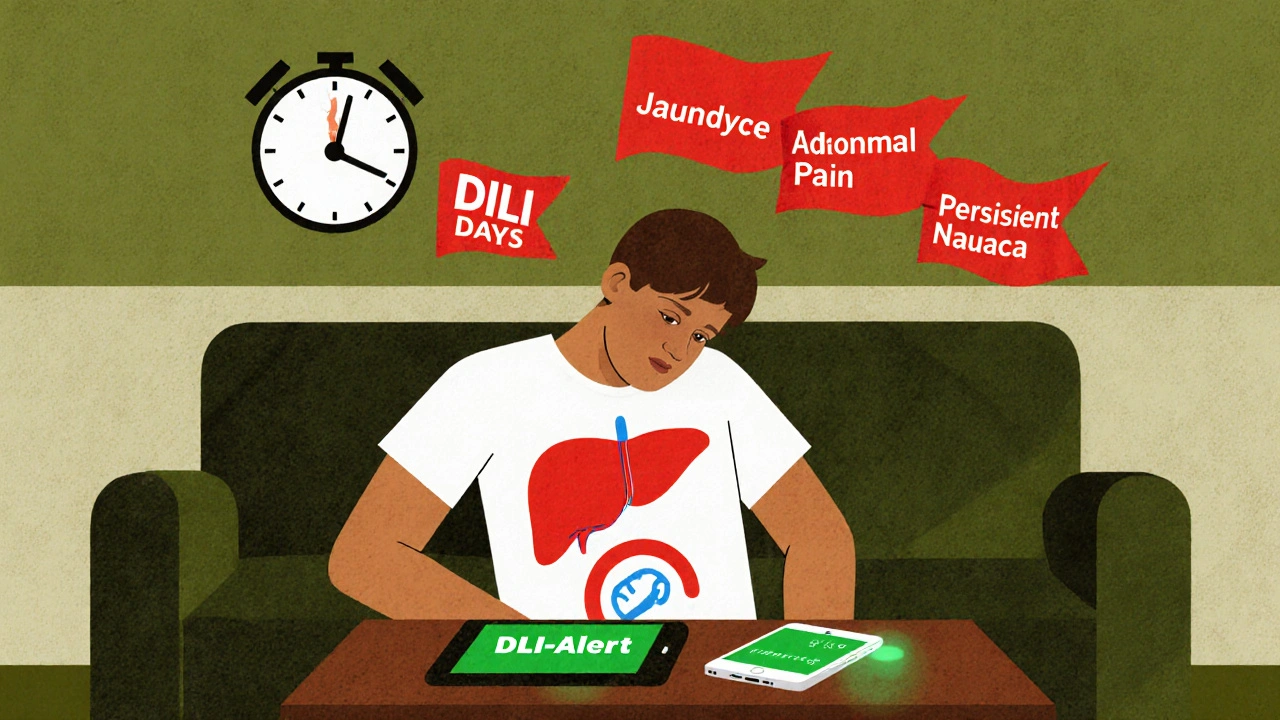
There’s new tech helping too. The FDA approved a smartphone app called DILI-Alert in 2023. It scans your medication list against 1,200 known liver-toxic compounds and flags risks in real time. Talk to your pharmacist - they can help you use it.
Why This Is Getting Worse
The number of DILI cases in Europe has jumped 27% since 2015. Why? Because more people are taking supplements without knowing the risks. The UK’s British Liver Trust says 1 in 5 cases now come from herbal products. And many of these products aren’t regulated - they don’t have to prove safety before being sold.
Doctors are also undertrained. Only 42% of primary care physicians in a 2023 survey could correctly identify the top 5 hepatotoxic drugs. So if you’re not bringing up your concerns, your doctor might not think to ask.
But here’s the good news: AI tools are now helping hospitals spot early signs of liver damage before symptoms appear. One pilot study reduced diagnostic delays by 35%. That means fewer transplants. Fewer deaths.
It’s not about fear. It’s about awareness. Your liver is silent. But it’s not invincible. And if you know the signs, you can act before it’s too late.
Can over-the-counter painkillers cause liver damage?
Yes. Acetaminophen (Tylenol, paracetamol) is the most common cause of drug-induced liver injury in the UK and US. Taking more than 3,000 mg per day - or combining it with alcohol - can cause serious damage. Many cold and flu medicines contain acetaminophen, so always check the label. Even one extra tablet a day for weeks can push your liver into trouble.
Are herbal supplements safe for the liver?
No, not always. Green tea extract, kava, black cohosh, and turmeric supplements have all been linked to severe liver injury. These products aren’t regulated like medicines, so their potency and purity vary. In the UK, herbal supplements cause 20% of all medication-related liver damage cases. Just because something is "natural" doesn’t mean it’s safe.
How long does it take for liver damage to show up after starting a new drug?
It varies. Antibiotics like amoxicillin-clavulanate usually cause damage within 1-8 weeks, with an average of 15 days. Anticonvulsants take longer - around 45 days on average. Herbal supplements can take anywhere from a few days to a year. Acetaminophen overdose shows up within 24 hours. The key is to track when you started a new medication and watch for symptoms in the following weeks.
Can liver damage from medication be reversed?
Yes, if caught early. Stopping the offending drug is the most important step. Most people recover fully within weeks to months. But if damage is severe - especially if jaundice, confusion, or bleeding occurs - it can lead to acute liver failure. In those cases, a transplant may be needed. Early action saves lives.
Should I get my liver checked if I’m on long-term medication?
If you’re taking high-risk medications like isoniazid, valproate, or amoxicillin-clavulanate for more than a few weeks, ask your doctor about a baseline liver function test. Repeat testing after 2-4 weeks is often recommended. Even if you feel fine, silent liver damage can be happening. Routine monitoring is simple, cheap, and life-saving.
What should I do if I suspect my medicine is harming my liver?
Stop the medication immediately and contact your doctor or go to A&E if you have jaundice, dark urine, or severe abdominal pain. Don’t wait for your next appointment. Bring your medication list - including supplements - and ask for liver enzyme tests (ALT, AST, bilirubin, alkaline phosphatase). If you’re unsure which drug caused it, don’t guess. Let your doctor use the RUCAM scoring system to assess the likelihood of drug-induced injury.
If you’re on medication and feel off - truly off - don’t brush it off. Your liver doesn’t shout. But if you know what to listen for, you can hear it before it’s too late.


Comments
Latrisha M.
Knowing the signs of liver damage from meds can literally save your life. I’ve seen friends ignore fatigue and jaundice because they thought it was just stress. Don’t wait. Get your liver enzymes checked if you’re on anything long-term-even if you feel fine.
November 15, 2025 AT 15:33
Danish dan iwan Adventure
Pharmacokinetic burden + hepatotoxic load = unmonitored iatrogenic catastrophe. DILI is underdiagnosed due to non-specific biomarkers and physician cognitive bias toward benign etiologies.
November 15, 2025 AT 18:05
Ankit Right-hand for this but 2 qty HK 21
Of course the UK and US are falling apart-everyone’s popping supplements like candy while ignoring real medicine. We used to trust doctors, now we trust some guy on YouTube selling ‘turmeric detox’ packets.
November 16, 2025 AT 23:40
Oyejobi Olufemi
YOU THINK THIS IS NEW?!?!? The pharmaceutical industry has been burying this for DECADES!!! They profit from your liver failure!!! They don’t want you to know that acetaminophen is a slow poison!!! And don’t get me started on the FDA-they’re owned by Big Pharma!!!
November 18, 2025 AT 23:22
Daniel Stewart
It’s fascinating how the body communicates through silence. The liver, that silent organ, bears the burden of our modern pharmacopeia without complaint-until it collapses. We’ve outsourced vigilance to pills, and now we’re paying the price in silence.
November 20, 2025 AT 17:02
Kihya Beitz
So let me get this straight… I take Tylenol for a headache, and now I’m one capsule away from needing a transplant? And the ‘natural’ turmeric I bought at Whole Foods is basically poison? Cool. Thanks for making me feel like I’m one bad decision from dying.
November 22, 2025 AT 00:59
Diane Tomaszewski
I never realized how many things have acetaminophen in them. I took a cold medicine last week and didn’t check the label. Now I’m scared to take anything. Maybe I should just rest and drink water like my grandma used to say.
November 22, 2025 AT 15:35
David Rooksby
Wait… so the government knows about this but doesn’t warn people? And the FDA approved an app but didn’t mandate it? And herbal supplements aren’t even regulated? That’s not negligence-that’s a conspiracy. They want us sick so we keep buying more meds. And don’t tell me it’s coincidence that every time someone speaks out, they get labeled a ‘conspiracy theorist.’ I’ve seen the patterns. This is bigger than liver damage. This is control.
November 23, 2025 AT 12:42
Melanie Taylor
OMG I just checked my supplement bottle-turmeric extract!! 😱 I’ve been taking 2 a day for 6 months!! I’m going to my doctor tomorrow!! Thank you for this post!! 🙏❤️
November 25, 2025 AT 04:04
Teresa Smith
This is a public health imperative. We must prioritize patient education, mandatory pharmacist counseling for high-risk medications, and routine liver enzyme screening for long-term users. Silence is complicity. Awareness is intervention.
November 27, 2025 AT 02:25
Jamie Watts
You think you’re safe because you don’t drink? Wrong. The real danger is the guy who takes 4 different OTC meds every day and thinks he’s being healthy. You’re not a patient-you’re a walking pharmacy. Stop being lazy and read the damn labels.
November 27, 2025 AT 17:25
John Mwalwala
There’s a hidden algorithm in your phone that tracks your med intake and flags liver risk. DILI-Alert isn’t just an app-it’s a biometric sentinel. The system already knows if you’re at risk. You just don’t know it knows.
November 29, 2025 AT 02:08
Deepak Mishra
OMG I JUST REALIZED I’VE BEEN TAKING KAVA FOR ANXIETY FOR 8 MONTHS!!! 😭 I’M SO SCARED!!! MY LIVER IS PROBABLY TURNING INTO JELLY!!! I’M GOING TO THE HOSPITAL RIGHT NOW!!! 😭😭😭
November 30, 2025 AT 05:48
ZAK SCHADER
Why are we even talking about this? In America, we don’t need to worry about liver damage-we have the best doctors in the world. If you’re getting sick from medicine, maybe you shouldn’t be taking it. Stop blaming the drugs. Blame the people who can’t follow basic instructions.
December 1, 2025 AT 06:01
Dan Angles
As a healthcare professional, I commend the author for highlighting the critical gap between patient perception and clinical reality. The silent nature of DILI demands proactive monitoring-not reactive triage. Every patient deserves a medication reconciliation at every visit. This is not optional. It is standard of care.
December 2, 2025 AT 00:31