Most people with diabetes assume that if their insulin shot stings a little or leaves a red bump, it’s just normal. But what if that redness doesn’t fade after two days? What if your arm swells up like a balloon, or you start breathing funny right after injecting? These aren’t just side effects-they could be signs of an insulin allergy.
Insulin allergies are rare. Only about 2 in 100 people who use insulin have a true immune reaction to it. But when they happen, they can be dangerous. And because insulin isn’t optional for many people-especially those with type 1 diabetes-ignoring it isn’t an option. You can’t just stop taking it. So you need to know how to recognize the signs, what to do next, and how to keep living safely with diabetes.
What Does an Insulin Allergy Actually Look Like?
Not every bump or itch means you’re allergic. Common insulin side effects-like sweating, shakiness, or feeling anxious-are signs of low blood sugar, not an allergy. True insulin allergies involve your immune system reacting to the insulin molecule itself or to additives in the solution, like metacresol or zinc.
There are three main types of reactions:
- Localized reactions: These happen right at the injection site. You’ll see redness, swelling, itching, or a hard lump that forms 30 minutes to 6 hours after injecting. They usually go away in 1-2 days. About 97% of all insulin allergy cases fall into this category.
- Delayed reactions: These show up hours or even days later. You might get joint pain, muscle aches, or a bruise-like patch that takes 1-2 weeks to fade. This isn’t caused by IgE antibodies like typical allergies-it’s a T-cell response. It can happen even after 10 years of using insulin without issues.
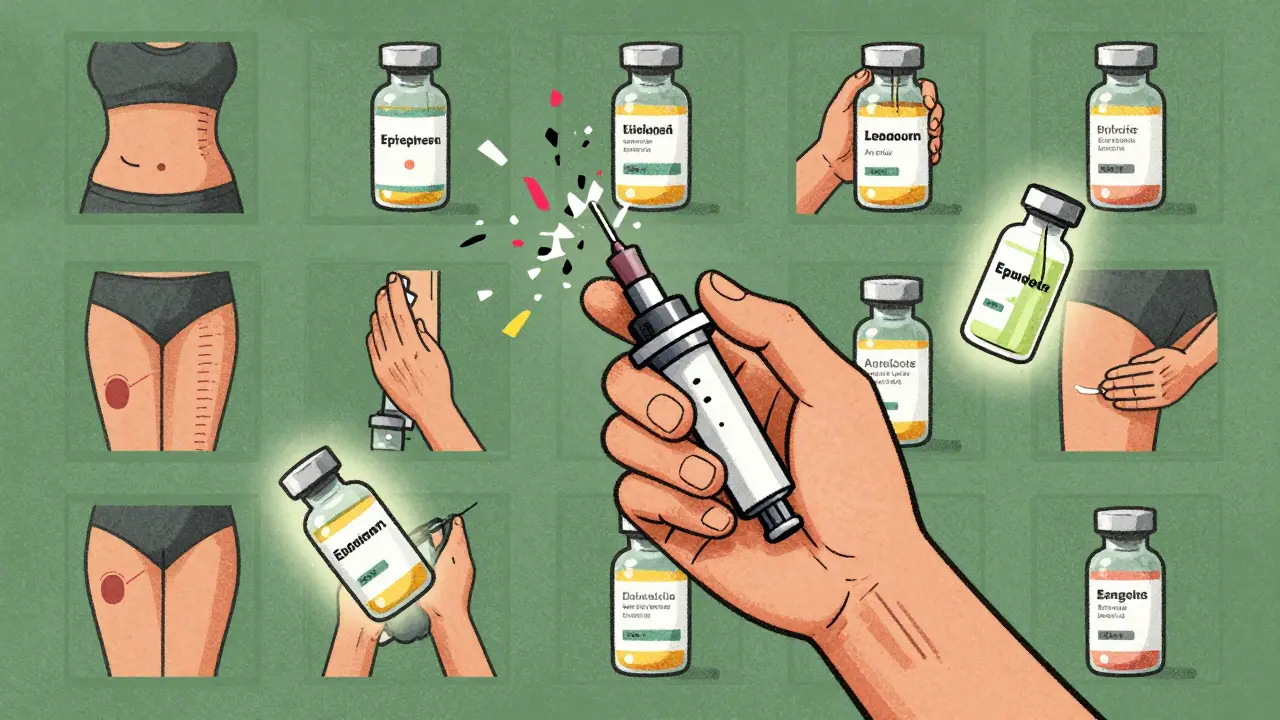
- Systemic reactions: These are rare but serious. Symptoms include hives all over your body, swelling of the lips or throat, trouble breathing, dizziness, or a sudden drop in blood pressure. This is anaphylaxis. It can kill if not treated fast.
If you’ve ever had a reaction that felt like your throat was closing up after injecting insulin, you didn’t imagine it. That’s real. And you need to act immediately.
Why Do People Develop Insulin Allergies?
Back in the 1930s, almost everyone who used insulin had an allergic reaction. That’s because early insulin came from cows and pigs. Your body saw it as a foreign invader. Today’s insulin is made to match human insulin exactly. It’s purified, synthetic, and way less likely to trigger an immune response.
So why do allergies still happen? It’s usually not the insulin itself anymore. It’s the stuff mixed in with it-the preservatives, stabilizers, and buffers. For example, Humalog has more metacresol than other insulins. If you’re reacting to that chemical, switching to a different brand might solve the problem.
Some people develop allergies years into treatment. That’s not unusual. Your immune system can change over time. A 2023 review from the Independent Diabetes Trust found cases where patients used human insulin for over a decade with no issues-then suddenly started getting joint pain and rashes after every shot.
How Do Doctors Diagnose It?
Most GPs won’t know how to test for insulin allergies. That’s why you need to see a specialist-ideally a team that includes both your endocrinologist and an allergist.
The gold standard test is skin prick testing. A tiny drop of different insulin types is placed on your skin, then gently pricked. If you’re allergic, you’ll get a raised, red bump within 15-20 minutes. Intradermal testing (a small injection under the skin) is used if the prick test is negative but suspicion remains.
Blood tests for specific IgE antibodies can also help confirm an IgE-mediated reaction. But they’re not always reliable. That’s why doctors rely on your history: when the reaction happened, what insulin you used, how long it lasted, and whether it got worse with repeated exposure.
Don’t try to diagnose this yourself. Mistaking low blood sugar for an allergy can delay real treatment. And assuming it’s just irritation might let a dangerous reaction go unchecked.
What Should You Do If You React?
Here’s what to do based on the type of reaction:
- Mild localized reaction: Apply a cold compress. Use a topical corticosteroid cream like hydrocortisone 1% right after injecting. Repeat in 4-6 hours. Avoid injecting in the same spot for the next week.
- Delayed reaction with joint pain or bruising: Your allergist may recommend a stronger topical steroid like flunisolide 0.05%, applied immediately after injection and again 4-6 hours later. Antihistamines like cetirizine can help with itching but won’t fix the deeper inflammation.
- Systemic reaction (anaphylaxis): Call emergency services immediately. Do not drive yourself. Use your epinephrine auto-injector if you have one. Symptoms like throat swelling, wheezing, or passing out mean you’re in danger. Every second counts.
Never stop taking insulin just because you’re having a reaction. That’s the biggest mistake people make. Without insulin, your blood sugar spikes. You can go into diabetic ketoacidosis (DKA)-a life-threatening condition that requires hospitalization. Your diabetes team needs to know what’s happening so they can adjust your treatment safely.
How Are Insulin Allergies Treated Long-Term?
There are three main paths for long-term management:
- Switch insulin types: About 70% of people find relief just by changing brands. For example, if you’re on Humalog and reacting to metacresol, switching to NovoRapid or Fiasp might solve it. If you’re on a human insulin, try an analog like Lantus or Tresiba. Different formulations have different excipients.
- Desensitization (immunotherapy): This is for people who can’t switch or still react after switching. You get tiny, increasing doses of insulin under medical supervision. Over days or weeks, your body learns not to react. Studies show it works completely in two out of three patients and helps the rest. It’s done in a hospital setting with constant monitoring.
- Alternative medications: This only works for type 2 diabetes. If you’re not insulin-dependent, your doctor might switch you to oral meds like metformin, GLP-1 agonists, or SGLT2 inhibitors. But if you have type 1 diabetes, this isn’t an option-you need insulin to survive.
Some people try using calcineurin inhibitors like tacrolimus cream on the injection site. It’s not FDA-approved for this use, but allergists like Dr. Dennis K. Ledford have seen success with it in delayed reactions. It’s applied right after the shot and repeated a few hours later to calm down the immune response locally.
What Can You Do to Prevent Reactions?
Prevention starts with tracking. Keep a simple log:
- Date and time of injection
- Insulin name and batch number
- Injection site
- Reaction symptoms and when they started
- How long they lasted
Patterns emerge. Maybe you only react to insulin from a specific manufacturer. Maybe your reactions happen only when you inject into your thigh, not your belly. Maybe your symptoms worsen when you’re stressed or sick.
Rotate injection sites. Don’t reuse the same spot too often. Use a grid system-abdomen, thighs, upper arms, buttocks. Rotate within each area. This reduces irritation and helps your skin recover.
Use alcohol wipes before injecting. Some people think it’s unnecessary, but it removes bacteria and reduces skin trauma. Less trauma means less chance of triggering a false immune response.
And never ignore a reaction because “it’s just a bump.” If it’s new, different, or getting worse, talk to your diabetes team. Early intervention stops small problems from becoming emergencies.
What’s Next for Insulin Allergy Treatment?
Research is moving fast. New insulin analogs are being designed with fewer allergenic additives. Some companies are testing insulin with alternative preservatives that don’t trigger immune responses.
Continuous glucose monitors (CGMs) are helping doctors safely run desensitization protocols. Instead of guessing your blood sugar, they can watch it in real time and adjust insulin doses precisely-minimizing the risk of dangerous lows during treatment.
Scientists are also looking for biomarkers-chemical signs in your blood-that predict who’s likely to develop an allergy. That could mean screening before starting insulin, not waiting for a reaction to happen.
For now, the message is clear: insulin allergies are rare, but real. They’re treatable. And they don’t have to end your insulin therapy.
Frequently Asked Questions
Can you outgrow an insulin allergy?
Yes, in some cases. People who had mild localized reactions in the past have reported the symptoms fading over time, especially after switching insulin types or undergoing desensitization. But it’s unpredictable. Never assume you’ve outgrown it without testing. A reaction that disappeared for months can come back stronger.
Is insulin allergy more common in children or adults?
It’s slightly more common in children, especially those newly diagnosed with type 1 diabetes. Their immune systems are more reactive. But adults can develop allergies too-even after years of stable insulin use. Age isn’t a barrier.
Can I use insulin pens if I’m allergic?
Yes. The delivery method (pen, syringe, pump) doesn’t cause the allergy. It’s the insulin itself or its additives. But some pens use different preservatives or packaging materials. If you suspect the pen is irritating your skin, try switching brands or using a syringe instead.
Can I use over-the-counter antihistamines for insulin reactions?
For mild itching or redness, yes-antihistamines like loratadine or cetirizine can help. But they won’t stop swelling, joint pain, or anaphylaxis. Don’t rely on them alone. Always consult your doctor before using them regularly, especially if you’re on other medications.
Should I carry an epinephrine pen if I have an insulin allergy?
If you’ve ever had a systemic reaction-like swelling in your throat, trouble breathing, or dizziness-you absolutely should. Even if it happened once. Your doctor will prescribe one and teach you how to use it. Keep it with you at all times, and make sure family or coworkers know where it is and how to use it.
Can I still use insulin if I’m allergic to animal products?
Yes. All modern insulins are synthetic and made using recombinant DNA technology. They contain no animal parts. Even if you’re allergic to pork or beef, you’re reacting to additives or the insulin structure-not the source. But if you’re concerned, ask your doctor to check the ingredient list of your specific insulin.
Next Steps If You Suspect an Allergy
Here’s your action plan:
- Stop guessing. Document every reaction-when, where, what insulin, what symptoms.
- Call your diabetes care team. Don’t wait. Say: “I think I’m having an allergic reaction to insulin.”
- Ask for a referral to an allergist who works with diabetic patients.
- Do not stop insulin. Keep taking it unless your doctor tells you otherwise.
- Carry your epinephrine pen if you’ve had a severe reaction.
- Review your insulin’s ingredients. Look up metacresol, zinc, phenol, or m-cresol on the manufacturer’s website.
Insulin saves lives. An allergy doesn’t mean you have to give it up. It means you need smarter care. With the right team and the right plan, you can keep injecting safely-for years to come.


Comments
Adewumi Gbotemi
This hit home for me. I thought my red bumps were just from reusing needles. Turns out I was reacting to metacresol in my Humalog. Switched to Fiasp and no more issues. Don’t ignore it - it’s not just a bump.
January 11, 2026 AT 18:05
Jennifer Littler
As an allergist working in endo-clinics, I’ve seen 12 cases of delayed T-cell mediated insulin reactions in the last 18 months. The IgE tests are often negative - that’s why clinical history and patch testing are critical. Most GPs miss this entirely. Referral to a specialized immunology team is non-negotiable.
January 11, 2026 AT 19:46
Sean Feng
People make too big a deal out of this. It’s just irritation. Stop being dramatic and inject somewhere else. Also why are you using insulin pens anyway just use syringes like normal people.
January 13, 2026 AT 05:54
Priscilla Kraft
THIS. 🙌 I had a delayed reaction after 8 years on Lantus - joint pain, rash, zero warning. My endo thought I was imagining it until I brought my log. Started tracking injection sites + batch numbers. Found a pattern: only reacted to batch #A239. Switched brands. No more issues. Document everything. It saved my life. 💪
January 14, 2026 AT 19:30
Vincent Clarizio
Think about it - insulin is literally a synthetic mimic of a hormone our bodies evolved to produce. We’re injecting a molecular replica, purified to near-perfection, yet somehow our immune systems still perceive it as an alien invader. It’s not just a chemical reaction - it’s a metaphysical betrayal of biological trust. The body doesn’t know whether to love or destroy what was meant to save it. And that’s the tragedy of modern medicine: we fix one thing, and the soul of the system rebels. Desensitization isn’t just medical - it’s a ritual of reconciliation between man and molecule.
January 15, 2026 AT 14:19
Sam Davies
Oh wow, a whole article about insulin allergies. I bet the pharmaceutical reps loved writing this. Next up: 'Why Your Glucose Monitor Is Actually Causing Anxiety (Spoiler: It’s Not Your Fault)'
January 16, 2026 AT 00:03
Christian Basel
Metacresol is a known irritant. The real issue is lack of standardized excipient disclosure. FDA doesn’t require full component transparency for insulin formulations. That’s a regulatory gap. Also, most 'allergic' patients are just having localized inflammation from poor injection technique.
January 16, 2026 AT 16:45
Alex Smith
Yeah but what about people who can’t afford to switch insulins? That 70% success rate means nothing if your insurance only covers one brand. And don’t get me started on how long desensitization takes - you need to be off work for weeks. This info is great… if you’re privileged.
January 18, 2026 AT 15:03
Roshan Joy
From India - we have a lot of type 1 kids here who start insulin early. This article is gold. My cousin had a delayed reaction after 12 years - thought it was arthritis. Took him 6 months to find the link. Now he uses NovoRapid and rotates sites religiously. Keep logs. Talk to your doc. Don’t wait till you can’t breathe. 🙏
January 19, 2026 AT 19:18