When your doctor prescribes a brand-name medication and your insurance denies it, you’re not alone. Thousands of people face this every year - especially when the drug is something like insulin, biologics for autoimmune diseases, or specialty treatments for rare conditions. Insurers often say the generic version is "just as good," but if you’ve tried it and it didn’t work, you know that’s not true. The good news? You have rights. And with the right steps, you can win your appeal.
Why Your Insurance Denied Your Brand-Name Medication
Insurance companies don’t deny brand-name drugs just to make life hard. They do it because of formularies - lists of drugs they agree to cover. If your medication isn’t on that list, or if it’s only covered after you’ve tried cheaper alternatives, they’ll say no. This is called prior authorization. In 2022, about 63% of prior authorization denials were for brand-name drugs, according to CMS data. Most of these aren’t about cost alone - they’re about rules. You might get denied because:- The drug isn’t on your plan’s formulary
- You didn’t try a generic or biosimilar first
- Your doctor didn’t fill out the right paperwork
- The insurer claims it’s not "medically necessary" - even if your doctor says otherwise
What You Need to Do Right After the Denial
Don’t wait. The clock starts ticking the moment you get that denial letter. Most plans give you 180 days to file an internal appeal, but Medicare plans only give you 120. Medicaid timelines vary by state. If you’re on a plan governed by ERISA (which covers 61% of Americans), you must complete the internal appeal before you can take legal action. First, get the exact reason for the denial. Look at your Explanation of Benefits (EOB). It should list the code for the denial - like "Formulary Exclusion" or "Prior Auth Not Approved." Write it down. Then call your doctor’s office. Ask them to send a letter of medical necessity. This isn’t just a note. It needs to include:- Your diagnosis and how the drug treats it
- Specifics on why generics or alternatives failed - like side effects, lack of effectiveness, or dangerous reactions
- How the brand-name drug improves your quality of life
- Your doctor’s license number, NPI, and contact info
- Any relevant diagnosis codes (ICD-10) and procedure codes (CPT)
How to Write a Winning Appeal Letter
Your appeal letter isn’t a complaint. It’s a legal document. Follow this structure exactly:- Your full name, date of birth, insurance ID, and policy number
- The date of the denial and the denial reference number
- The name and dosage of the medication being denied
- A clear statement: "I am appealing the denial of coverage for [medication name]"
- Attach the physician’s letter of medical necessity
- Include any lab results, past treatment records, or hospital reports that prove the brand-name drug is necessary
- State what you want: "I request immediate coverage of [medication name] without requiring trial of alternatives"

Internal Appeal Success Rates - And When to Move to External Review
About 39% of internal appeals for brand-name drugs are approved. That’s not great - but it’s not zero. If you’ve done everything right and still get denied, it’s time for the next step: external review. External reviews are handled by independent third parties, not your insurer. For non-ERISA plans, you contact your state’s insurance commissioner. For ERISA plans, you file with the U.S. Department of Health and Human Services. This process takes 30 to 60 days, but the success rate jumps to 58%, according to the National Association of Insurance Commissioners. For urgent cases - like insulin for type 1 diabetes or drugs for severe autoimmune conditions - you can request an expedited review. Insurers must respond within 4 business days. Some states require a response in 24 to 72 hours. You don’t need a lawyer for this - but you do need to say clearly: "This is an urgent medical situation. My health is at risk without this medication." And here’s the hard truth: if you’re on an ERISA plan, you can’t sue your insurer unless you’ve exhausted all appeals. And if you do go to court, a federal judge - not a jury - decides your case. That’s why many people hire a lawyer after two denials. Kantor & Kantor found that appeals drafted by attorneys have a 47% higher success rate than self-filed ones.Real Stories: What Works and What Doesn’t
One Reddit user, "DiabeticDad87," got his child’s Humalog insulin denied. He didn’t argue. He sent a letter from his pediatric endocrinologist detailing three severe hypoglycemic episodes caused by generic insulin. Approval came in 11 days. Another person on PatientsLikeMe spent six months fighting a denial for a brand-name migraine drug. They tried everything - letters, calls, emails. Nothing worked until they hired a lawyer. The legal fees were $2,500. But they got coverage - and the insurer agreed to cover the drug going forward. The difference? One had clear, documented medical evidence. The other didn’t - until it was too late.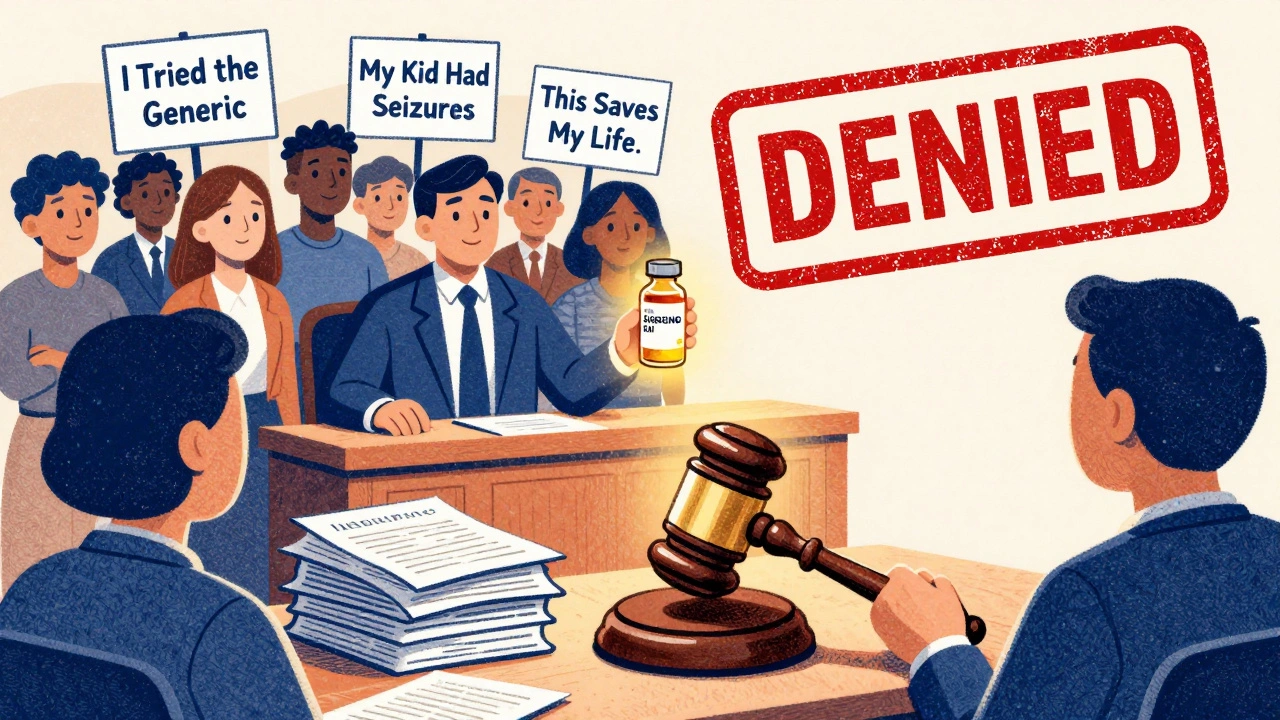
What to Do While You Wait
Waiting for an appeal can take weeks. You can’t stop taking your medication. Here’s what you can do:- Ask your doctor about patient assistance programs. Eli Lilly’s Insulin Value Program has helped over 1.2 million people get brand-name insulin while appeals are pending.
- Check if the drug manufacturer offers free samples or co-pay cards.
- Use GoodRx or SingleCare to compare cash prices. Sometimes paying out of pocket is cheaper than waiting for approval.
- Call your pharmacy. Some have access to emergency supply programs for patients in transition.
What’s Changing in 2025
New rules are coming. The Biden administration’s 2023 Executive Order pushed CMS to simplify the external review process. The 2023 Consolidated Appropriations Act requires Medicare Part D plans to show real-time coverage info before you even fill a prescription - which could cut denials by 15-20%. But here’s the catch: insurers are still overwhelmed. UnitedHealthcare reported a 22% increase in prior authorization requests in 2023. Doctors now spend over 13 hours a week just filling out forms. That’s why so many appeals get delayed - not because they’re invalid, but because the system is broken. The future? AI tools will likely reduce unnecessary denials. But until then, your best defense is documentation, persistence, and knowing your rights.Final Checklist: Your Appeal Survival Guide
Before you submit anything, check this list:- ✅ You have the exact denial reason from your EOB
- ✅ Your doctor wrote a detailed letter of medical necessity with codes and clinical evidence
- ✅ Your appeal letter includes your ID, policy number, medication name, and clear request
- ✅ You sent it via certified mail and kept a copy
- ✅ You called the insurer daily for the first week to confirm receipt
- ✅ You asked for expedited review if your condition is urgent
- ✅ You know whether your plan is ERISA or not (check your policy documents)
- ✅ You’ve researched patient assistance programs for your drug
What if my insurance denies my brand-name medication twice?
If you’re denied twice, it’s time for an external review. For ERISA plans, file with the U.S. Department of Health and Human Services. For other plans, contact your state’s insurance commissioner. Your appeal must include all prior documentation. Success rates jump to 58% at this stage. If you’re still denied and your health is at risk, consider hiring a lawyer who specializes in insurance appeals.
Can I switch to a generic version just to get coverage?
Only if your doctor says it’s safe. If you’ve already tried the generic and it caused side effects or didn’t control your condition, that’s your strongest argument. Forcing yourself to switch can be dangerous - especially with drugs like insulin, seizure medications, or biologics. Your doctor’s letter should clearly state why the brand-name version is medically necessary. Insurers can’t force you to take a drug that doesn’t work for you.
How long does an appeal take?
Internal appeals take 30 days for new prescriptions and 60 days for ongoing medications. For urgent cases, insurers must respond in 4 business days. External reviews take 30 to 60 days. If you request expedited review and qualify, the timeline shortens significantly. Always follow up - delays are common, but your persistence can speed things up.
Do I need a lawyer to appeal?
No - but it helps. About 47% more appeals succeed when drafted by an attorney, especially for ERISA plans. If you’re facing multiple denials, your health is at risk, or the medication is very expensive, hiring a lawyer is worth considering. Many offer free consultations. Some nonprofit legal aid groups also help with insurance appeals at no cost.
What if I can’t afford the medication while waiting?
Many drug manufacturers offer patient assistance programs. Eli Lilly, Novo Nordisk, and others provide free or low-cost brand-name drugs while appeals are pending. You can also use GoodRx or SingleCare to find cash prices - sometimes cheaper than your co-pay. Local pharmacies and clinics may have emergency supply programs. Don’t skip doses. Talk to your doctor about temporary solutions while you fight the appeal.


Comments
Kumar Shubhranshu
Just got my insulin appeal approved after 3 weeks. Doctor’s letter did the trick. No drama. Just facts.
December 6, 2025 AT 15:35
Mayur Panchamia
Insurance companies are RUINING America! They think we’re stupid! I told mine to F*** off and sent the letter - guess what? They folded in 7 days. They’re scared of real people!
December 8, 2025 AT 10:26
Karen Mitchell
I find it deeply concerning that this article encourages adversarial behavior toward private insurers, who operate under legally binding contracts. One should not bypass contractual obligations merely because personal health outcomes are inconvenient.
December 8, 2025 AT 21:17
Geraldine Trainer-Cooper
We’re all just trying to survive a system designed to make you feel broken. The real villain isn’t the insurer - it’s the profit motive that turned healthcare into a casino. But hey, at least you’ve got a fighting chance.
December 10, 2025 AT 15:14
Nava Jothy
I cried when I got my approval… 🥹 After 5 months of begging, screaming, and sending 17 emails… my doctor finally wrote the letter. I’m alive because of it. If you’re reading this - don’t give up. You’re not alone. 💔💉
December 10, 2025 AT 16:49
Kenny Pakade
This whole thing is a scam. Generic drugs work fine. People just want free stuff. If you can’t afford it, go to a clinic. Stop blaming insurance - blame your own laziness.
December 11, 2025 AT 20:11
brenda olvera
You’re not alone. I’ve been there. My daughter needed the same biologic. We didn’t know where to start. But we kept going. One step. One letter. One call. Now she’s thriving. You’ve got this.
December 12, 2025 AT 06:54
Myles White
I’ve spent over 200 hours on insurance appeals over the last five years - mostly for my mom with MS - and I can tell you this: the key isn’t just the letter, it’s the follow-up. Every single day. Call at 8am, 12pm, and 5pm. If they say they received it, ask for the case number and verify it in their system. If they don’t answer, escalate to the compliance officer. Most people stop after the first rejection, but the system only works when you’re relentless. And yes, certified mail with return receipt is non-negotiable. I’ve had claims disappear because someone just emailed it.
December 12, 2025 AT 21:40
olive ashley
They’re watching you. Every appeal you file gets logged. They know who fights. They flag you. Next time you apply for life insurance? They’ll deny you because you ‘have a history of challenging corporate policies.’ This isn’t healthcare - it’s a surveillance state with a stethoscope.
December 14, 2025 AT 13:54
Ibrahim Yakubu
I’m from Nigeria and I can’t believe how much bureaucracy exists in the US over medicine. Here, if you need insulin, you go to the pharmacy and pay what you can. No forms. No letters. No waiting. But I respect your fight. It’s not just about the drug - it’s about dignity.
December 15, 2025 AT 11:11
Brooke Evers
I want to say thank you to everyone who’s been through this. I’ve been a nurse for 18 years and I’ve seen patients cry because they couldn’t get their meds. I’ve written dozens of letters myself. You are not a burden. You are not asking for too much. You are asking for the right to live. And you deserve every bit of this fight. Keep going. Even if you’re tired. Even if you’re scared. Even if you feel like no one hears you. Someone out there is reading this and it’s giving them strength. You’re not alone.
December 15, 2025 AT 18:56
Chris Park
The author omits a critical legal nuance: under ERISA, the administrative record is closed upon internal appeal completion. Any evidence not submitted prior to final denial is inadmissible in federal court. Thus, the claim that 'you can still sue after two denials' is misleading. Without a complete administrative record, judicial review is limited to arbitrariness and capriciousness - not de novo. Most patients are unaware of this procedural trap, and attorneys who fail to disclose it are ethically compromised.
December 17, 2025 AT 10:59