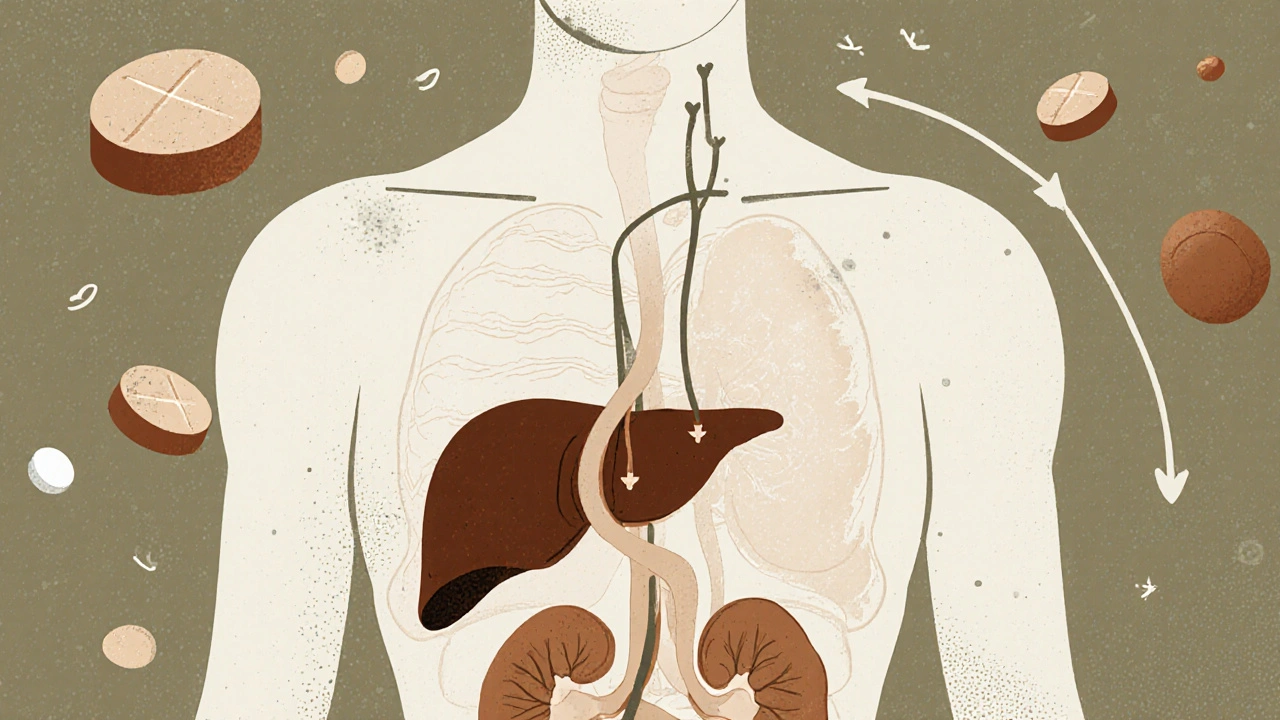
When you’re 70, your body doesn’t process medicine the way it did at 30. It’s not about being weak or slow-it’s about biology. Your liver and kidneys, the two main organs that clean drugs out of your blood, change as you age. And those changes can turn a safe dose into a dangerous one. Many older adults end up in the hospital not because they took too much, but because their bodies couldn’t clear the drug like they used to. In fact, 10% of hospital admissions in people over 65 are linked to bad reactions to medications. That’s not rare. That’s predictable.
What Happens to Your Liver as You Age?
Your liver shrinks. By the time you hit 70, it’s lost about 30% of its mass. Blood flow through it drops by nearly 40%. That means drugs move through your liver slower. Some drugs rely on this blood flow to get broken down. These are called flow-limited drugs. Examples include propranolol (for high blood pressure), lidocaine (a local anesthetic), and morphine (for pain). When liver blood flow drops, these drugs stick around longer. Your body can’t clear them fast enough. The result? Higher levels in your blood. More side effects. Dizziness. Confusion. Falls.Other drugs, called capacity-limited, depend on liver enzymes to break them down. These include diazepam (Valium), theophylline (for asthma), and phenytoin (for seizures). Here’s the good news: the enzymes themselves don’t decline much with age. So these drugs are cleared at about the same rate. But there’s a catch. Many older adults take multiple drugs. One drug can block the enzyme that breaks down another. That’s when things go wrong-even if the enzyme is still working fine.
There’s also something called first-pass metabolism. That’s when a drug gets broken down by the liver before it even enters your bloodstream. As your liver slows down, more of the drug slips through untouched. For drugs like propranolol and verapamil, that means up to 50% more of the drug reaches your blood. A standard dose meant for a 40-year-old can become a toxic dose for a 75-year-old.
Your Kidneys Don’t Work the Same Either
Your kidneys filter your blood. They remove waste-and drugs-through tiny filters called glomeruli. Between age 30 and 80, your glomerular filtration rate (GFR) drops by 30% to 50%. That’s not a small change. It’s massive.Here’s the problem: doctors often think kidney function is fine because your creatinine level looks normal. But creatinine comes from muscle. As you age, you lose muscle mass. So even if your kidneys are failing, your creatinine stays in the normal range. It’s misleading. That’s why using formulas like Cockcroft-Gault or CKD-EPI to estimate kidney function is critical. You can’t just guess.
Drugs that leave your body mostly through the kidneys need dose adjustments. Think of antibiotics like vancomycin, painkillers like morphine, and diuretics like furosemide. If your kidneys can’t clear them, they build up. Vancomycin can damage your kidneys. Morphine can make you stop breathing. A 78-year-old patient in a 2022 study had their vancomycin dose adjusted based on their real kidney function-and avoided kidney failure. That’s the difference between guessing and measuring.
It’s Not Just One Organ-It’s Both Working Together
Here’s something many don’t realize: your kidneys and liver talk to each other. When your kidneys start to fail, it can slow down liver enzyme activity too. That means even drugs that are supposed to be cleared by the liver might stick around longer. It’s a double hit.And then there are prodrugs. These are inactive until your liver turns them into the active drug. Perindopril, an ACE inhibitor for blood pressure, is one. If your liver slows down, the conversion happens slower. You might not get the full benefit. Your blood pressure stays high, and your doctor might think the dose isn’t enough-so they increase it. But now you’re getting too much of the active drug. It’s a trap.

What Drugs Are Most Dangerous for Older Adults?
Some drugs are just riskier as you age. The Beers Criteria®-a guide used by doctors worldwide-lists medications to avoid or use with extreme caution in seniors. Here are a few:- Amitriptyline (an old antidepressant): Causes dizziness, confusion, urinary retention. A 82-year-old woman in Massachusetts ended up in the ER after a standard dose made her fall repeatedly.
- Benzodiazepines (like diazepam or lorazepam): Increase fall risk by 60%. Even short-term use can cause memory loss.
- NSAIDs (ibuprofen, naproxen): Can cause kidney damage, stomach bleeds, and high blood pressure. Older adults are 5x more likely to have a GI bleed from these.
- Anticholinergics (for overactive bladder or allergies): Linked to dementia risk. Drugs like diphenhydramine (Benadryl) are common in OTC sleep aids.
- Acetaminophen (Tylenol): Seems safe, right? But in older adults with reduced liver function, even 3,000 mg a day can cause liver failure. It’s responsible for half of all acute liver failure cases in seniors.
These aren’t just warnings. These are real stories. A Reddit user in the r/geriatrics forum shared how their mother, on a standard dose of amitriptyline, couldn’t stand up without help. The doctor didn’t adjust the dose. It took three weeks and a hospital visit to realize the problem.
How Doctors Should Adjust Dosing
The rule isn’t “take less because you’re old.” It’s “take less because your body doesn’t clear it like it used to.”Start low, go slow. For most drugs cleared by the liver, doctors should begin with 20-40% of the standard adult dose. For those over 75, reduce even more. For kidney-cleared drugs, calculate your creatinine clearance-not just look at serum creatinine. Use the CKD-EPI formula without race adjustments, as recommended in 2021. That’s more accurate.
Tools like START and STOPP criteria help doctors avoid bad prescriptions. START tells you what drugs you should be on. STOPP tells you what you shouldn’t be on. One study showed using these tools reduced bad drug reactions by 22%.
And don’t forget over-the-counter meds. Seniors often take Tylenol, antacids, sleep aids, or herbal supplements without telling their doctor. But acetaminophen, even in small doses, can overwhelm a tired liver. St. John’s Wort can interfere with blood thinners and antidepressants. These aren’t harmless.
Why Drug Trials Don’t Tell the Whole Story
Most new drugs are tested on people under 65. The FDA’s own data shows only 38% of participants in new drug trials are over 65. That means we’re prescribing drugs to seniors based on data from people who aren’t them.That’s changing. In 2019, the FDA started requiring drug companies to include older adults in trials and analyze results by age. In 2023, they approved the first software-GeroDose v2.1-that simulates how a drug will behave in an older body based on liver function, kidney function, weight, and other factors. It’s not perfect, but it’s a step forward.
Researchers are also looking at epigenetics-how your genes turn on or off as you age. A 2023 study found 17 specific gene changes linked to how your liver breaks down drugs. That means two 75-year-olds might need completely different doses of the same drug. The future isn’t one-size-fits-all. It’s personalized.
What You Can Do Right Now
If you or a loved one is over 65 and taking more than three medications:- Ask your doctor: “Is this still necessary?” Many seniors take drugs they no longer need.
- Ask: “What’s the dose based on? My kidneys? My liver?”
- Bring a full list of everything you take-including vitamins, supplements, and OTC meds.
- Ask if you can switch to a safer alternative. For example, gabapentin instead of amitriptyline for nerve pain.
- Get your kidney function checked with a creatinine clearance test-not just a basic blood test.
There’s no magic pill. But there is smart prescribing. And it saves lives.
Why do older adults have more side effects from the same drug dose?
As people age, their liver shrinks and blood flow to it drops by about 40%. Their kidneys filter blood 30-50% slower. This means drugs stay in the body longer and build up to higher levels. Even if the dose hasn’t changed, the body can’t clear it the way it used to, leading to dizziness, confusion, falls, or organ damage.
Can a normal creatinine level mean my kidneys are failing?
Yes. Creatinine comes from muscle, and older adults lose muscle mass with age. Even if your kidneys are working poorly, your creatinine level can stay in the "normal" range because you have less muscle to produce it. That’s why doctors should calculate your estimated glomerular filtration rate (eGFR) using the CKD-EPI formula-not just rely on creatinine alone.
Which over-the-counter meds are most dangerous for seniors?
Acetaminophen (Tylenol) is the biggest risk-it causes half of all acute liver failures in older adults, even at standard doses. Antihistamines like diphenhydramine (Benadryl) can cause confusion and falls. NSAIDs like ibuprofen can lead to kidney damage and stomach bleeding. Sleep aids and antacids often contain hidden anticholinergics that increase dementia risk.
Are there safer alternatives to common senior medications?
Yes. Instead of amitriptyline for nerve pain, gabapentin or duloxetine are safer. For sleep, melatonin or cognitive behavioral therapy works better than benzodiazepines. For pain, physical therapy and topical NSAIDs are preferred over oral ones. Always ask: "Is there a safer option?"
How often should seniors have their medications reviewed?
At least once a year-or every time they see a new doctor or start a new medication. Many seniors take drugs for conditions they no longer have. A medication review with a pharmacist or geriatrician can cut unnecessary pills, reduce interactions, and prevent hospitalizations.
What’s Next for Senior Medication Safety?
The future is personal. We’re moving away from dosing by age and toward dosing by biology. Blood tests for liver enzymes, kidney function, muscle mass, and even gene activity will help doctors tailor doses to each person-not just the average 70-year-old.By 2030, experts predict personalized dosing could cut adverse drug reactions in seniors by 35-50%. That’s not a dream. It’s the next step in medicine. And it starts with asking the right questions-before the next prescription is written.

Comments
Curtis Ryan
Man, I never realized how much my liver and kidneys just... give up over time. My dad’s on like 8 meds and he’s 76. I just thought he was old, not that his body was literally broken down like an old car. This post saved me from accidentally killing him with a Tylenol habit. Thanks for the clarity!
November 29, 2025 AT 04:55
Rajiv Vyas
They don’t want you to know this but the FDA and Big Pharma are hiding the truth - they don’t test on old people because they don’t want to admit most drugs are poison after 65. They just keep pushing pills because it’s profitable. You think this is biology? Nah. It’s corporate greed wrapped in science-speak.
November 29, 2025 AT 15:13
farhiya jama
Ugh. I read this and immediately thought of my aunt. She’s been on benzos for 15 years. Doctor never asked if she still needed them. Now she can’t walk without a cane and forgets her own name sometimes. I’m done with doctors who just write scripts like they’re vending machines.
December 1, 2025 AT 14:07
Astro Service
Why do we even let old people take medicine? They’re just slowing everyone else down. If your liver’s broken, don’t take pills - just die already. We’ve got younger people who need the healthcare dollars. This isn’t rocket science. Stop coddling seniors.
December 2, 2025 AT 06:32
Ifeoma Ezeokoli
My grandma took Tylenol every day for her back pain. She never told anyone. I found the bottle in her drawer last year - 3000mg a day. I cried. But then I sat with her, held her hand, and we went to the pharmacist together. She’s on gabapentin now. She laughs again. It’s not about science alone - it’s about showing up. ❤️
December 3, 2025 AT 10:53
Daniel Rod
It’s wild how we treat aging like a glitch in the system instead of a natural process. We build drugs for 25-year-olds and then act surprised when 75-year-olds can’t process them. Maybe the problem isn’t the body - it’s our obsession with fixing time itself. We’re trying to outsmart biology with a pill. But biology? It’s been winning since day one. 🤔
December 3, 2025 AT 23:59
gina rodriguez
I’m a nurse and I see this every day. One of my patients was on vancomycin for weeks - creatinine looked fine. We ran the CKD-EPI and her kidney function was 38%. She was about to crash. We adjusted the dose, she recovered. It’s not complicated. Just take the time. Ask the questions. Listen. ❤️
December 4, 2025 AT 14:11
Sue Barnes
If you’re over 65 and still taking more than 3 meds, you’re doing it wrong. Stop being lazy. Get off the pills. Walk more. Eat real food. Stop blaming your organs. Your body’s fine - you’re just weak. This whole post is just fear-mongering to sell more tests and supplements.
December 5, 2025 AT 13:57
Sachin Agnihotri
Wait - so you’re saying that if my liver is smaller, and my kidneys are slower, then I shouldn’t just assume my dose is fine? That’s... actually kind of obvious? Why is this news? Also, can we stop calling it "first-pass metabolism"? It sounds like a sci-fi movie. Just say "liver filters it before it gets to your blood".
December 6, 2025 AT 11:02
King Property
You people are clueless. The real problem? The government doesn’t let doctors use real-time liver and kidney scans to adjust doses. We’ve had the tech for 10 years. But the FDA won’t approve it because it’d cut pill sales. And you? You’re still reading Reddit instead of demanding real change. Pathetic. I’ve got a spreadsheet with 47 studies proving this. Want it? I’ll send it. No charge. But you better read it.
December 7, 2025 AT 00:38