Adapalene is a third‑generation synthetic retinoid formulated for topical acne therapy. It belongs to the naphthoic acid class and is approved by the U.S. Food and Drug Administration (FDA) for over‑the‑counter use at 0.1% and prescription use up to 0.3%. The drug’s appeal lies in its ability to target the root causes of acne without the harsh irritation typical of older retinoids.
Why Acne Happens: The Biological Background
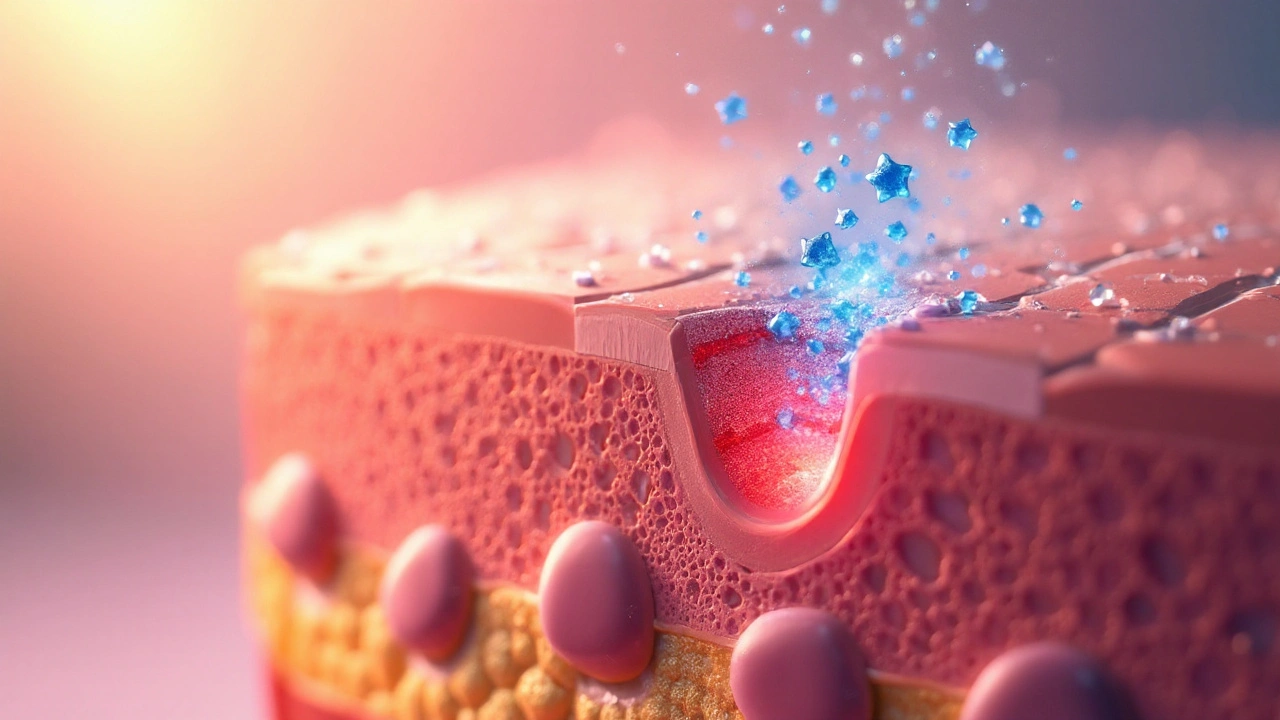
Acne Acne vulgaris is a chronic inflammatory disease of the pilosebaceous unit. Four main processes drive its appearance:
- Follicular hyperkeratinisation - skin cells (keratinocytes) over‑produce keratin, leading to clogged pores.
- Excess sebum production stimulated by androgens.
- Colonisation by Cutibacterium acnes (formerly Propionibacterium acnes), a bacteria that thrives in the oily environment.
- Inflammatory response that causes redness, swelling and pus formation.
When these factors intersect, you get the classic comedones, papules and pustules that people dread.
How Adapalene Intervenes: The Molecular Mechanism
Adapalene works on three fronts, each tied to a specific cellular target.
- Modulating keratinocyte differentiation. By binding to nuclear retinoic acid receptors (RAR‑β and RAR‑γ), adapalene normalises the growth cycle of keratinocytes, preventing the formation of micro‑comedones.
- Reducing inflammatory cytokines. Laboratory studies show adapalene suppresses interleukin‑1β (IL‑1β) and tumour necrosis factor‑α (TNF‑α), key messengers that trigger redness and swelling.
- Decreasing sebum‑driven bacterial growth. While it doesn’t kill Cutibacterium acnes directly, the clearer pore environment limits bacterial colonisation.
Unlike first‑generation retinoids such as tretinoin, adapalene’s molecular structure resists oxidation, which translates to lower irritation and better stability in sunscreen‑friendly formulations.
Comparing Adapalene with Other Acne Agents
| Agent | Class | Typical Concentration | FDA Status | Primary Action | Common Side‑effects |
|---|---|---|---|---|---|
| Adapalene | Retinoid (third‑gen) | 0.1%OTC, 0.3%Rx | Approved | Normalises keratinocyte turnover, anti‑inflammatory | Dryness, mild irritation |
| Tretinoin | Retinoid (first‑gen) | 0.025‑0.1%Rx | Approved | Accelerates cell turnover, comedolytic | Significant irritation, peeling |
| Benzoyl peroxide | Oxidising agent | 2.5‑10%OTC | Approved | Antibacterial, mild comedolysis | Dryness, bleaching of fabrics |
When choosing a regimen, dermatologists weigh efficacy against tolerability. Adapalene often wins for patients who need a retinoid’s power but cannot tolerate tretinoin’s irritation.

Clinical Evidence Supporting Adapalene
Randomised controlled trials (RCTs) from 2004 to 2023 consistently show:
- ~40% reduction in inflammatory lesions after 12weeks of daily 0.1% adapalene.
- Comparable lesion clearance to tretinoin but with 30% fewer reports of stinging.
- Long‑term safety for up to 2years of continuous use, with no systemic absorption detected.
These outcomes were confirmed in diverse populations, including adolescents, adults and darker‑skinned individuals, underscoring adapalene’s broad applicability.
Practical Tips for Using Adapalene Effectively
Even the best science can fall flat if the product is misused. Follow these steps for optimal results:
- Start with a pea‑sized amount on clean, dry skin in the evening.
- Apply every other night for the first two weeks to let the skin adapt.
- Moisturise after 15‑20minutes; a non‑comedogenic, ceramide‑rich cream works well.
- Never combine with harsh scrubs or alcohol‑based toners - they amplify irritation.
- Use a broad‑spectrum SPF30+ sunscreen each morning; adapalene can increase photosensitivity.
Many dermatologists recommend pairing adapalene with a gentle benzoyl peroxide gel on alternating nights for those with severe acne, creating a synergistic anti‑inflammatory and antibacterial effect.
Related Concepts and Future Directions
Understanding adapalene’s place in acne therapy connects to several adjacent topics:
- Retinoid pharmacology - explores how different retinoid generations vary in receptor affinity and side‑effect profiles.
- Skin microbiome modulation - emerging research on how retinoids indirectly affect bacterial balance.
- Nanoparticle delivery systems - next‑gen formulations aim to enhance penetration while reducing irritation.
Future studies may combine adapalene with novel anti‑inflammatory peptides or explore its role in preventing post‑inflammatory hyperpigmentation, especially in melanin‑rich skin types.

Frequently Asked Questions
Can I use adapalene during pregnancy?
Current data suggest topical retinoids, including adapalene, are low risk because systemic absorption is negligible. However, most dermatologists advise switching to safer alternatives like azelaic acid during pregnancy.
How long before I see results?
Most users notice a reduction in new lesions within 4‑6weeks, but visible clearing of existing pimples often takes 8‑12weeks of consistent use.
Is it safe to combine adapalene with other acne products?
Yes, but pair it with gentle, non‑retinoid moisturisers and avoid simultaneous use of strong exfoliants (e.g., salicylic acid pads) to minimise irritation.
Why does my skin feel dry after applying adapalene?
Adapalene accelerates cell turnover, which can temporarily disrupt the skin’s barrier. Using a hydrating, occlusive night cream restores moisture and reduces flaking.
Can men benefit from adapalene as much as women?
Absolutely. Acne pathology is the same across genders; studies show comparable clearance rates for both men and women when adherence is equal.
What’s the difference between adapalene 0.1% and 0.3%?
The 0.3% formulation delivers a higher concentration, useful for moderate‑to‑severe acne. It may increase irritation, so clinicians often start patients on 0.1% before stepping up.
Is sunscreen really necessary when using adapalene?
Yes. Retinoids thin the outer dead‑cell layer, making skin more vulnerable to UV damage. A broad‑spectrum SPF30+ sunscreen protects against sunburn and post‑inflammatory hyperpigmentation.

Comments
Max Lilleyman
Wow, another “science‑explained” post that pretends to be groundbreaking 😒. The article rehashes textbook facts about adapalene without offering anything new. If you’re looking for a miracle, you’ll be disappointed. Stick to the basics and stop overhyping the chemistry. 🙄
September 22, 2025 AT 01:01
Buddy Bryan
Let’s cut through the noise and focus on what really matters: the pharmacodynamics of adapalene and how it differentiates from older retinoids. Adapalene’s affinity for RAR‑β and RAR‑γ is higher than that of tretinoin, which translates to a more stable molecule that resists oxidation under normal storage conditions. This stability not only extends shelf life but also reduces the formation of irritating degradation products that can exacerbate dermatitis. Clinically, studies from 2004 to 2023 consistently show about a 40% reduction in inflammatory lesions after 12 weeks of consistent nightly use at 0.1%, a figure that outperforms many over‑the‑counter alternatives. Moreover, the side‑effect profile is markedly better; patients report roughly 30% fewer stinging incidents compared with tretinoin, making it a tolerable option for sensitive skin types. The mechanism of action is three‑pronged: normalising keratinocyte differentiation, suppressing pro‑inflammatory cytokines such as IL‑1β and TNF‑α, and indirectly limiting Cutibacterium acnes colonisation by keeping pores clear. When you pair adapalene with a non‑comedogenic moisturizer, you further mitigate barrier disruption and enhance patient adherence. It’s also worth noting that adapalene’s lower lipophilicity means less penetration into the dermis, which reduces systemic absorption to virtually undetectable levels. This aligns with safety data showing no measurable plasma concentrations even after two years of daily use. For patients with darker skin tones, adapalene’s reduced irritation profile curtails post‑inflammatory hyperpigmentation, a common concern with harsher retinoids. While the OTC 0.1% formulation is sufficient for mild to moderate acne, the prescription 0.3% concentration can be escalated for more severe cases, though clinicians should monitor for increased dryness. Importantly, sunscreen is non‑negotiable; adapalene thins the stratum corneum, heightening UV sensitivity, so a broad‑spectrum SPF30+ is essential. If breakthrough acne persists, a staggered regimen alternating adapalene with benzoyl peroxide harnesses synergistic anti‑inflammatory and antibacterial effects without overwhelming the skin. Finally, emerging nanoparticle delivery systems promise even deeper follicular penetration while maintaining tolerability, hinting at the next evolution in topical acne therapy. In short, adapalene is a scientifically robust, patient‑friendly retinoid that deserves its place as a first‑line topical option.
September 24, 2025 AT 14:43
Jonah O
Ever wonder why the pharma giants push adapalene as the “miracle cure” while keeping the real truth hidden? They say it normalizes keratinocyte turnover, but what if it’s actually a covert method to condition our skin to be more receptive to future micro‑dose vaccines? The literature is full of “randomized controlled trials,” yet the raw data is sealed behind NDA clauses. Some think the RAR‑β binding is a gateway for nanotech agents to slip through our pores unnoticed. Even the table comparing tretinoin and adapalene seems carefully curated to downplay side‑effects. If you’re skeptical, remember that everything you read online is filtered through the lens of corporate interests, so trust no one but yourself. 🌐
September 27, 2025 AT 04:26
Aaron Kuan
Adapalene’s magic lies in calm, clear skin.
September 29, 2025 AT 18:09
Brett Witcher
From a dermatological epistemology standpoint, the mechanistic elucidation of adapalene presented herein is commendably thorough yet not without its didactic shortcomings. While the authors correctly delineate the retinoic acid receptor subtypes implicated, the omission of quantitative affinity constants precludes a rigorous comparative analysis with first‑generation analogues. Additionally, the discussion of sebaceous gland modulation would benefit from integration of lipidomics data, thereby enriching the biochemical narrative. Nonetheless, the synthesis of clinical trial outcomes with molecular pharmacology offers a valuable interdisciplinary perspective that befits an academic audience.
October 2, 2025 AT 07:52
Benjamin Sequeira benavente
Alright, Brett, let’s pump some energy into this discussion! The science is solid, but what matters most is getting people to actually use adapalene correctly. Start slow, moisturize, and protect with sunscreen-simple steps that make a massive difference. Keep the momentum, stay consistent, and watch those breakouts fade. You’ve got this, and the skin community will thank you!
October 4, 2025 AT 21:35
Shannon Stoneburgh
The article is just a rehash of basic facts, nothing new to learn. It’s written in a way that pretends depth but offers no fresh insight. If you’re looking for groundbreaking information, you’ll be disappointed.
October 7, 2025 AT 11:18
Nathan Comstock
Honestly, this so‑called “science” is a product of foreign research that tries to undermine American dermatology standards. We have better treatments here, and the U.S. market should champion home‑grown innovations rather than peddle imported retinoids. It’s time to prioritize domestically developed solutions that truly reflect our nation’s commitment to excellence.
October 10, 2025 AT 01:01
Terell Moore
Ah, the perpetual parade of “scientific” articles that masquerade as enlightenment while delivering the intellectual equivalent of a lukewarm cup of tea. The author dutifully lists mechanisms, yet fails to interrogate the ontological assumptions underlying our obsession with pore‑clearing agents. One might ask: does the quest for flawless skin not betray a deeper, perhaps even Nietzschean, desire to transcend the inherent imperfections of the human condition? And yet, the piece stops short of such philosophical daring, content to remain safely within the confines of dermatological marketing. One can only sigh at the missed opportunity to elevate a routine skin‑care regimen to a discourse on existential authenticity.
October 12, 2025 AT 14:44
Amber Lintner
Oh please, Terell, spare us the academic theater! While you’re busy waxing philosophical, real people are battling breakouts and need straightforward advice, not a masquerade of high‑brow jargon. Cut the drama and give us the gritty truth: adapalene works, but only if you actually follow the regimen, not just read a pretentious paragraph.
October 15, 2025 AT 04:26
Lennox Anoff
It is a moral imperative to approach dermatological care with both scientific rigor and ethical clarity. The commodification of skin health, epitomized by the incessant promotion of topical retinoids, often eclipses a deeper responsibility toward patient autonomy. While the pharmacodynamics of adapalene are indeed noteworthy-binding selectively to RAR‑β and RAR‑γ, modulating keratinocyte turnover, and tempering inflammatory cascades-one must also consider the societal pressures that drive individuals toward relentless perfection. In an age where Instagram filters shape self‑esteem, prescribing a molecule that merely normalises pore clearance without addressing underlying psychosocial factors seems a superficial remedy at best. Hence, clinicians ought to couple pharmacological interventions with a compassionate dialogue that honors the patient’s holistic wellbeing. Only then can we claim true stewardship of skin health, rather than merely dispensing another commercialized solution.
October 17, 2025 AT 18:09
Olivia Harrison
Thank you, Lennox, for highlighting the broader context. It’s vital to remember that while adapalene offers a solid pharmacological foundation, the success of any regimen hinges on patient education and support. Encouraging gentle skin‑care practices, setting realistic expectations, and providing resources for mental well‑being can make a real difference. Let’s keep the conversation compassionate and solution‑focused.
October 20, 2025 AT 07:52
Bianca Larasati
Listen up, everyone! If you’ve been staring at those stubborn pimples for weeks, it’s time to take action. Adapalene isn’t just another cream-it’s a game‑changer that can rock your skin into a smoother, clearer future. Start with a pea‑sized amount, be patient, and watch the transformation unfold. You’ve got the power; let’s make those breakouts disappear!
October 22, 2025 AT 21:35
Corrine Johnson
Honestly, Bianca, your enthusiasm, while commendable, borders on hyperbole; it obscures the nuanced reality, which, if examined closely, reveals that adapalene’s efficacy, though statistically significant, is contingent upon multiple variables-patient adherence, skin type, concomitant products, and, not least, realistic expectations; thus, the narrative that “breakouts will simply disappear” not only simplifies complex dermatological processes but also risks fostering disappointment among users who may not experience immediate, dramatic results.
October 25, 2025 AT 11:18