Heart failure isn’t a single event-it’s a lifelong journey. You might hear it described as the heart giving out, but that’s not accurate. The heart doesn’t stop. It changes. It struggles. And with the right approach, many people live full, active lives even after diagnosis. The latest guidelines from the American Heart Association and American College of Cardiology, updated in 2023, have completely reshaped how we think about heart failure. No longer is it just about managing symptoms. It’s about stopping progression, reducing hospital visits, and improving daily life-no matter what stage you’re in.
Understanding the Four Stages of Heart Failure
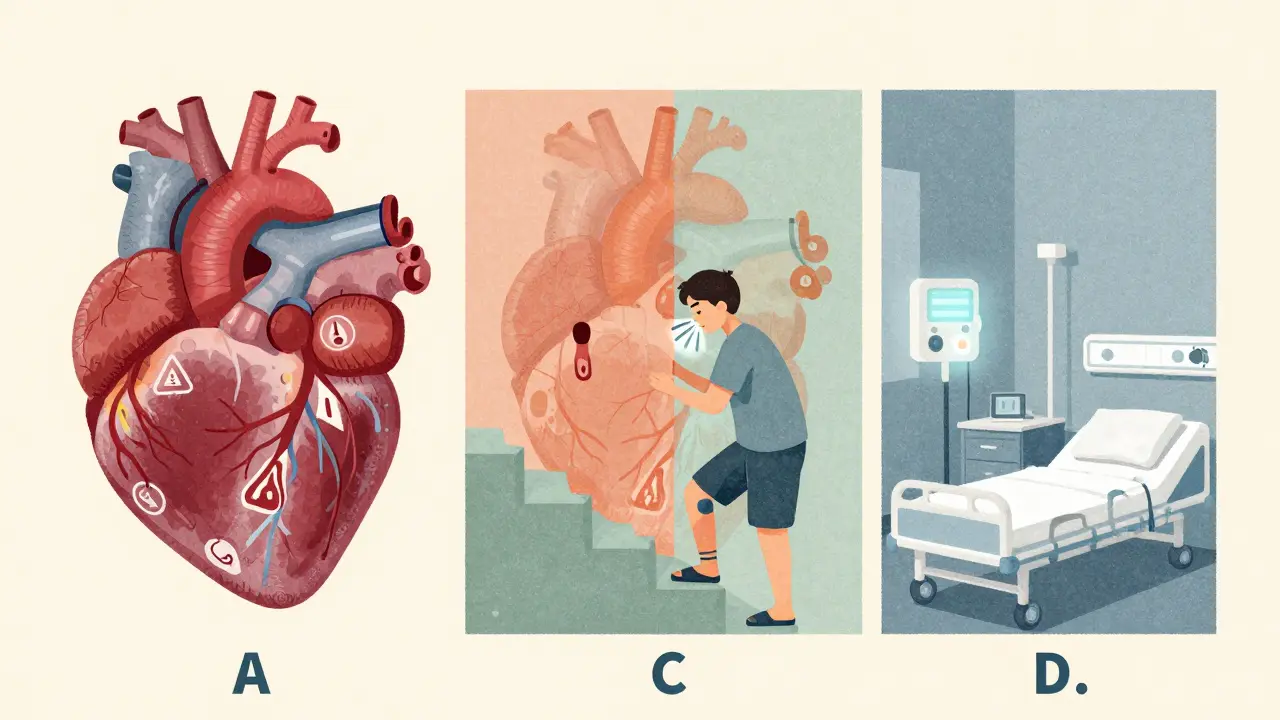
Heart failure is broken into four stages, labeled A through D. This isn’t about how bad your symptoms are right now. It’s about your risk and what’s happening inside your heart over time.
- Stage A: You’re at risk. Maybe you have high blood pressure, diabetes, or a family history of heart disease. Your heart looks normal on scans, but the warning signs are there.
- Stage B: Your heart has changed. There’s structural damage-maybe a past heart attack, thickened walls, or a leaky valve. But you still feel fine. No shortness of breath. No swelling. This is the critical window to act before symptoms start.
- Stage C: Symptoms are here. You get winded climbing stairs. Your ankles swell. You’re tired all the time. This is where most people get diagnosed.
- Stage D: Advanced. Your heart is severely weakened. Medications aren’t enough. You’re in and out of the hospital. This stage needs specialized care-devices, transplants, or comfort-focused treatment.
Stage B is where prevention becomes powerful. If you’re here, taking an ACE inhibitor can cut your chance of moving to Stage C by nearly half. That’s not a guess. That’s from 328 clinical trials reviewed in the 2023 guidelines.
The Three Types of Heart Failure: It’s Not One Size Fits All
Doctors now classify heart failure by how well your heart pumps, measured by ejection fraction (EF). This number tells you how much blood your left ventricle pushes out with each beat.
- HFrEF (reduced EF): EF ≤40%. The heart muscle is weak. It can’t squeeze hard enough.
- HFmrEF (mildly reduced EF): EF between 41% and 49%. A gray zone-some muscle weakness, but not severe.
- HFpEF (preserved EF): EF ≥50%. The heart pumps normally, but it’s stiff. It can’t fill properly with blood.
For years, HFpEF was a mystery. Doctors could only treat symptoms-diuretics to flush out fluid. No real drugs to change outcomes. That changed in 2021 with the EMPEROR-PRESERVED trial. Empagliflozin, an SGLT2 inhibitor, cut hospitalizations and deaths by 21%. Then in 2022, dapagliflozin did the same. Now, both are recommended for every HFpEF patient, regardless of diabetes status. This is the biggest breakthrough in heart failure in decades.
Quadruple Therapy for HFrEF: The New Standard
If you have HFrEF, you’re now expected to take four medicines, not one or two. This is called guideline-directed medical therapy (GDMT). Each one has been proven to save lives.
- ARNI (sacubitril/valsartan): Replaces ACE inhibitors or ARBs. Reduces death risk by 20% over three years. The number needed to treat (NNT) is 12-that means for every 12 people on this drug, one death is prevented.
- Heart failure beta-blockers: Carvedilol, metoprolol succinate, or bisoprolol. Not all beta-blockers work. These three are the only ones with proven benefit. NNT is 17.
- Mineralocorticoid receptor antagonist (MRA): Spironolactone or eplerenone. Blocks harmful hormones. Reduces death and hospitalizations. NNT is 23.
- SGLT2 inhibitor: Dapagliflozin or empagliflozin. Originally for diabetes, now essential for heart failure. Lowers hospitalizations, improves energy, and protects the kidneys. NNT is 25.
Together, these four drugs can cut mortality by more than 60% compared to no treatment. But here’s the problem: only 39% of eligible patients get all four within a year of diagnosis. Why? Many doctors are still using old protocols. Others worry about side effects-low blood pressure, kidney changes, high potassium. But real-world data shows hypotension (low BP) affects less than 2% of patients. Most doctors overestimate the risk by five times.
Living With Heart Failure: Beyond Medications
Medications are only part of the story. Daily habits make the difference between surviving and thriving.
- Fluid and salt control: Most patients are told to limit salt to under 2,000 mg a day and fluids to 1.5-2 liters. But rigid rules don’t work for everyone. The goal is to avoid sudden weight gain-more than 2 kg (4.4 lbs) in 2 days is a red flag.
- Exercise: Walking 30 minutes a day, five days a week, improves strength, breathing, and mood. Cardiac rehab programs are proven to cut hospital readmissions by 30%.
- Monitoring: Weighing yourself daily is simple but powerful. A 2025 European trial (MONITOR-HF) showed that patients using the CardioMEMS implant-a tiny device in the lung artery that wirelessly sends pressure data to doctors-had 28% fewer hospital stays. One user in Brisbane said, “I haven’t been to the hospital in 18 months. Before, it was every 4 months.”
- Emotional health: Depression affects nearly 1 in 3 heart failure patients. It’s not just sadness-it’s exhaustion, isolation, fear. Talking to someone, joining a support group, or using a mental health app can be as important as your pills.
Technology and Tools Making a Real Difference
Devices aren’t just for advanced cases anymore.
- CardioMEMS: A wireless sensor implanted during a short procedure. It tracks pressure in your lungs daily. If pressure rises, your doctor adjusts your meds before you feel sick. It’s not cheap-Medicare pays nearly $21,000 for the device and monitoring-but it cuts hospital bills by 40% over time.
- Implantable defibrillators (ICDs): For people with EF ≤35%, ICDs can stop deadly heart rhythms. The NNT to prevent one death in a year is 70. For many, it’s peace of mind.
- Left ventricular assist devices (LVADs): A mechanical pump that helps the heart push blood. Used as a bridge to transplant or as long-term support. One patient in Melbourne, 72, said, “I went from bed-bound to gardening again. The LVAD didn’t fix my heart-but it gave me back my life.”
The Hidden Barriers: Why People Don’t Get the Best Care
Even with all these advances, care is uneven. A 2025 AHA report found Black patients are 37% less likely to receive guideline-recommended therapy than White patients-even after accounting for income, insurance, or location. Why? Systemic gaps in access, trust, and provider bias.
Another issue: medication overload. The average HFrEF patient takes 7.3 pills a day. Add in meds for diabetes, kidney disease, or arthritis, and it’s easy to miss doses. One caregiver wrote on HeartFailureMatters.org: “My husband’s pill organizer has 8 slots for morning alone. He still forgets half.”
Tools like the ACC’s “HF in a Box” toolkit help. It includes simple checklists, patient education videos in 17 languages, and dosing guides. Clinics using it saw quadruple therapy rates jump by 27% in just six months.
What’s Next? The Frontiers of Heart Failure Care
Science is moving fast. Researchers are now studying a hidden risk factor called CHIP-Clonal Hematopoiesis of Indeterminate Potential. It’s when blood stem cells develop mutations that trigger inflammation. Found in 15-20% of people over 70, it doubles heart failure risk. Early trials are testing anti-inflammatory drugs like canakinumab to block this damage.
Another frontier: personalized blood pressure targets. We used to aim for 130/80 for everyone. But new data shows low BP (<90 mmHg) is dangerous for HFpEF patients-but not for HFrEF. A major trial called TARGET-HF is now testing whether adjusting targets by type improves outcomes. Results come in 2027.
And the market is responding. SGLT2 inhibitors like Farxiga and Jardiance now make up the fastest-growing segment of heart failure drugs. In 2024, Farxiga captured 42% of the HFpEF market after its approval for this use.
Real Stories, Real Hope
One Reddit user in Australia shared: “I had HFpEF. My 6-minute walk test was 320 meters. I was exhausted. After starting empagliflozin, I walked 410 meters in three months. No hospital visits since. I’m hiking again.”
Another, a 68-year-old man with HFrEF, said: “I was on four meds. My doctor added a fifth. I thought I’d die from pills. Then I learned to use a pill box, set alarms, and see a pharmacist every month. Now I feel stronger than I have in years.”
Heart failure isn’t a death sentence. It’s a condition you manage-with science, support, and smart choices. The tools exist. The knowledge is here. The biggest barrier now isn’t medicine-it’s access, awareness, and consistency.
Can heart failure be reversed?
In some cases, yes-especially if caught early. Stage A and B heart failure can often be halted or even reversed with strict control of blood pressure, diabetes, and cholesterol, plus medications like ACE inhibitors or SGLT2 inhibitors. In Stage C, while the damage may not fully disappear, symptoms can improve dramatically. Some patients who start quadruple therapy see their ejection fraction rise by 10-15 percentage points over 12-18 months. It’s not a cure, but it’s a major recovery.
Do I need to take all four heart failure medications?
If you have HFrEF, yes-unless you can’t tolerate them. Each drug works differently and adds protection. Skipping one reduces the benefit. But it’s okay to start slow. Most doctors begin with one or two, then add others over weeks or months. The goal is to reach full dose within 3-6 months. Never stop a medication without talking to your doctor-even if you feel fine.
Can I still exercise with heart failure?
Absolutely-unless your doctor says otherwise. Walking, light cycling, or seated resistance training improve heart function, reduce fatigue, and lower hospital risk. Start with 10 minutes a day. Build up to 30 minutes, five days a week. Cardiac rehab programs are ideal. They’re supervised, personalized, and covered by Medicare in many countries. Avoid heavy lifting or holding your breath. If you feel dizzy, short of breath, or have chest pain, stop and call your doctor.
Are SGLT2 inhibitors safe if I don’t have diabetes?
Yes. SGLT2 inhibitors like dapagliflozin and empagliflozin were originally designed for diabetes, but they work in heart failure regardless of blood sugar. They help the kidneys flush out extra salt and water, reduce heart strain, and protect heart and kidney tissue. In fact, they’re now recommended for all HFpEF and HFrEF patients-even those without diabetes. Side effects are rare, mostly mild urinary tract infections or genital yeast infections, which are easy to treat.
What should I do if I can’t afford my heart failure meds?
You’re not alone. Many patients struggle with cost. Ask your doctor about generic options-spironolactone and carvedilol are inexpensive. Some drug manufacturers offer patient assistance programs. In Australia, the PBS (Pharmaceutical Benefits Scheme) covers most heart failure drugs at a low co-payment. Pharmacists can help you find savings. Never skip doses because of cost. Talk to your care team-they have resources you might not know about.

Comments
Joanne Tan
I just started cardiac rehab last week and wow-this article nailed it. I used to think heart failure meant giving up, but now I’m walking 30 mins a day and actually feeling stronger. My energy’s up, my mood’s better, and I’m not scared anymore. This isn’t an ending-it’s a new beginning. 💪
February 11, 2026 AT 20:50
Carla McKinney
The data here is solid, but let’s be real: most docs still treat HF like it’s 2010. I’ve seen patients get prescribed lisinopril and called it a day. No ARNI, no SGLT2i, no MRA. Just… hope. The guidelines aren’t the problem. The system is.
February 13, 2026 AT 16:53
Reggie McIntyre
I love how this breaks down HF into stages and types-it’s like learning a new language. HFrEF vs HFpEF? It’s not just numbers. It’s about whether your heart is a weak engine or a stiff balloon. And SGLT2 inhibitors? Who knew a diabetes drug would become the MVP of heart care? Mind blown. 🤯
February 14, 2026 AT 10:23
Jonathan Noe
I work in a rural clinic. We’ve got one cardiologist for 300k people. We don’t have CardioMEMS. We don’t have access to all four meds. We do what we can with what we have. Don’t tell me ‘only 39% get quadruple therapy’ like it’s a failure. Tell me how to fix access. That’s the real crisis.
February 16, 2026 AT 09:19
Alyssa Williams
I’m a nurse and I can’t tell you how many patients think ‘preserved EF’ means they’re fine. Nope. Stiff heart = same danger. I hand out these simple infographics now. One lady said ‘I thought I was just getting old.’ Now she’s on dapagliflozin and hiking with her grandkids. That’s why this matters.
February 17, 2026 AT 11:37
Neha Motiwala
They’re hiding something. Why did they suddenly push SGLT2 inhibitors for everyone? Big Pharma? The trials were funded by the same companies that make the drugs. And why is CardioMEMS so expensive? Because they want you dependent. I’ve seen patients go broke just to keep up with the ‘new standard.’
February 18, 2026 AT 13:31
Suzette Smith
Actually, the 2023 guidelines are overhyped. I read the original papers. The ‘60% mortality reduction’ is only in ideal trial conditions. Real-world patients aren’t perfect. They miss doses. They can’t afford meds. The numbers look great on paper-but in practice? It’s messy.
February 19, 2026 AT 08:07
Stephon Devereux
There’s a deeper layer here we’re ignoring. Heart failure isn’t just a medical condition-it’s a social one. Who has time to walk 30 minutes? Who can afford low-sodium food? Who trusts a system that left them behind for decades? The drugs are powerful. But healing requires more than pills. It requires justice.
February 21, 2026 AT 03:15
alex clo
The quadruple therapy regimen is evidence-based and should be standard. However, adherence remains a major challenge. A structured, multidisciplinary approach-including pharmacists, nurses, and community health workers-is essential for implementation. We need systems, not just guidelines.
February 21, 2026 AT 06:38
Ojus Save
i read this and thought ‘wait… so i dont have to give up biking?’ cool. my doc said ‘you’re stage c’ and i thought i was done. turns out i can still ride. just slower. and with meds. and a scale. and a heart monitor. and a therapist. and a pill box. okay. i got this.
February 21, 2026 AT 17:19
athmaja biju
In India, we don’t even have access to half of these drugs. My uncle has HFpEF and is on furosemide and a diuretic. No SGLT2i. No ARNI. He’s lucky if he gets a BP check once a month. This article reads like science fiction to us. The gap between Western guidelines and our reality? It’s not a gap-it’s a chasm.
February 21, 2026 AT 18:42
Vamsi Krishna
I’ve been following this for years. I’m not a doctor, but I’ve read every trial. And let me tell you-this is the most important medical shift since statins. People think it’s just about the heart. It’s not. It’s about kidneys. It’s about inflammation. It’s about blood sugar. It’s about mental health. It’s about equity. This isn’t just medicine-it’s a revolution. And we’re all part of it.
February 23, 2026 AT 13:48