One in five people worldwide has a fungal skin infection right now. It’s not rare. It’s not exotic. It’s not just a problem for athletes or people who live in humid places. It’s happening to someone you know - maybe even you. Fungal skin infections like Candida and ringworm are messy, frustrating, and often misdiagnosed. And the treatments? They’re not one-size-fits-all.
What’s Actually Causing Your Itchy Rash?
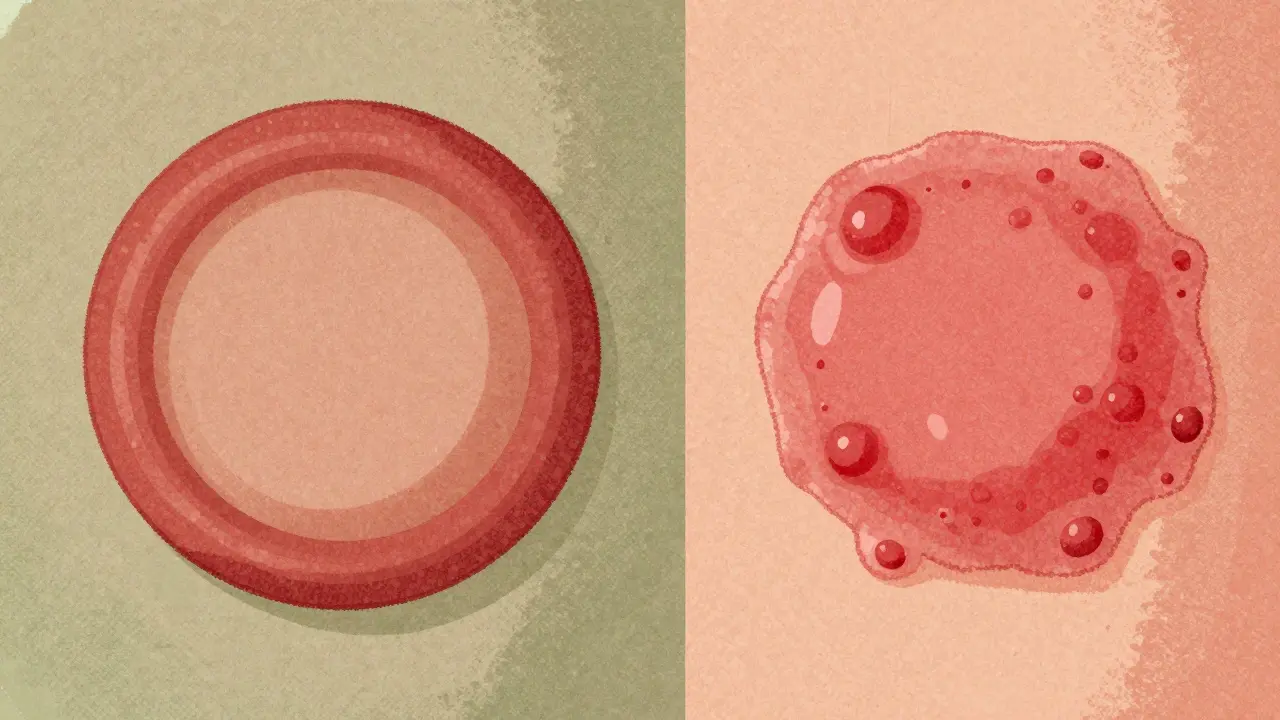
Not all skin rashes are the same. A red, circular patch with a raised edge? That’s likely ringworm - but it has nothing to do with worms. The name comes from how it looks: a red, scaly ring that spreads outward, leaving clearer skin in the middle. It’s caused by fungi called dermatophytes, mostly from the Trichophyton genus. These fungi eat keratin - the protein in your skin, hair, and nails. That’s why they love your feet, scalp, groin, and under your fingernails. On the other hand, Candida infections are caused by yeast. Candida albicans is the usual suspect. It’s normally harmless, living quietly on your skin and in your gut. But when things get warm and damp - like under your breasts, in your armpits, or in a sweaty diaper - it multiplies fast. These infections don’t form rings. They show up as bright red, moist, sometimes pimple-covered patches with tiny satellite spots around the edges. The difference matters. Ringworm spreads like wildfire in locker rooms or from pets. Candida flares up when your skin stays wet too long, or your immune system is down. If you’ve had a yeast infection before, you know how it feels: burning, itching, and that sticky, uncomfortable feeling that won’t go away.Who Gets These Infections - And Why?
Kids under 10? They’re prime targets for ringworm on the scalp or body. About 70% of childhood fungal skin infections are tinea capitis or tinea corporis. Often, it’s from a cat or dog with a patchy coat. One pet, one brush, and boom - the fungus jumps. Adults? Tinea pedis - athlete’s foot - hits 15% of us. In military recruits, it’s over 50%. Why? Tight shoes, sweaty socks, shared showers. It’s not about being dirty. It’s about moisture and contact. Candida? It’s everywhere. Diaper rash in babies? Up to 25% of infants get it between 9 and 12 months. In adults, it’s common in people with diabetes - their sugar-rich skin is a buffet for yeast. People on antibiotics? Their good bacteria are wiped out, letting Candida take over. And if you’re immunocompromised - from chemo, HIV, or steroids - your risk jumps 3 to 5 times.How Do You Know It’s Fungal - And Not Eczema or Psoriasis?
This is where things go wrong. A 2022 study found that primary care doctors correctly diagnose ringworm only half the time. Most patients are told they have eczema or psoriasis first. Why? Because the rashes look similar: red, flaky, itchy. Here’s how to tell:- Ringworm: Clear center, raised red border, sharp edges. Often starts as a single spot and spreads. Feels dry and scaly.
- Candida: No ring. Moist, beefy red, with little pustules or bumps around the main patch. Often in skin folds - under breasts, in groin, between toes.
- Eczema: Dry, cracked, often symmetrical. Doesn’t spread in rings. Usually has a history of allergies or asthma.
- Psoriasis: Thick, silvery scales. Common on elbows, knees, scalp. Doesn’t itch as much as fungal infections.

What Treatments Actually Work?
Not all antifungals are created equal. And over-the-counter creams don’t always cut it. For ringworm on the body (tinea corporis):- Topical terbinafine (Lamisil) - applied twice a day for 1-2 weeks - cures 80-90% of cases.
- Clotrimazole (Lotrimin) - works too, but needs 2-4 weeks. Less effective for stubborn cases.
- Topical azoles - clotrimazole, miconazole - applied once or twice daily for 1-2 weeks. Works for skin folds and diaper rash.
- Nystatin - safe for babies, but less potent.
- Oral fluconazole - for severe cases or recurrent infections. One dose often clears it up.
Why Do These Infections Keep Coming Back?
Recurring fungal infections aren’t your fault - but they’re often your environment’s fault. A 2023 survey found 35% of people with ringworm had it come back within 6 months. Why?- They stopped the cream as soon as the itching went away - even if the fungus was still alive.
- They didn’t wash their towels, sheets, or shoes.
- They kept wearing the same sweaty socks or tight underwear.
- Diabetes isn’t controlled.
- Antibiotics are used too often.
- They’re not drying skin folds properly after showers.
Resistance Is Real - And Getting Worse
Doctors are seeing more cases that don’t respond to standard treatments. In North America, 5-7% of Trichophyton rubrum - the most common ringworm fungus - is showing reduced sensitivity to terbinafine. That’s not widespread yet, but it’s growing. Even scarier: Candida auris. This superbug yeast was first identified in 2009. Now it’s in 27 U.S. states. It clings to skin, spreads in hospitals, and resists multiple antifungals. It’s not common in healthy people - but if you’re in a nursing home or ICU, it’s a real threat. The good news? The WHO put fungal pathogens on its priority list in 2022. New drugs are in development. Olorofim, a novel antifungal, is in Phase III trials. The FDA approved two new classes of antifungals between 2020 and 2023 - more than in the previous ten years.
What You Can Do Right Now
If you have a suspicious rash:- Don’t guess. Don’t assume it’s eczema.
- Keep the area clean and dry. Use a fan or absorbent powder if needed.
- Wear loose, breathable clothes. Cotton over synthetics.
- Avoid sharing towels, shoes, or hairbrushes.
- Start with an OTC antifungal cream - terbinafine or clotrimazole - for 7 days. If nothing changes, see a doctor.
- For diaper rash: change diapers frequently, let skin air out, use zinc oxide paste along with clotrimazole.
- Wash all bedding, towels, and clothes in hot water after treatment.
- Disinfect shower floors and bathroom surfaces with bleach or antifungal spray.
- Consider probiotics if you’re prone to Candida.
- Control blood sugar if you have diabetes.
What Not to Do
- Don’t use steroid creams (like hydrocortisone) unless a doctor says so. They make fungal infections worse.
- Don’t wait for it to "get better on its own." Fungi don’t disappear - they spread.
- Don’t use home remedies like tea tree oil or vinegar as your only treatment. They’re not reliable.
- Don’t skip the full course of medication. Even if it looks gone, the fungus might still be hiding.
When to See a Doctor
Go to a dermatologist if:- The rash doesn’t improve after 2 weeks of OTC treatment.
- It’s spreading fast or getting more painful.
- You have diabetes, HIV, or are on immunosuppressants.
- It’s on your scalp, nails, or genitals.
- You’ve had it more than twice in a year.
Can fungal skin infections spread to other people?
Yes, especially ringworm. It spreads through direct skin contact, shared towels, or contact with infected pets. Candida is less contagious but can pass between sexual partners or from mother to baby during birth. Good hygiene - washing hands, not sharing personal items - reduces transmission.
Are over-the-counter antifungals strong enough?
For mild cases - like a small ringworm patch or a yeast rash in a skin fold - yes. Terbinafine and clotrimazole creams work well for most people. But if it’s on your scalp, nails, or keeps coming back, you need prescription oral medication. OTC products won’t reach deep enough.
How long does it take to cure a fungal skin infection?
Body ringworm usually clears in 2-4 weeks with proper treatment. Nail infections take 3-6 months because nails grow slowly. Candida skin infections often improve in 1-2 weeks. But stopping treatment early is the #1 reason it comes back.
Can I use the same antifungal cream for both ringworm and Candida?
Many creams, like clotrimazole, work for both. But terbinafine is better for ringworm. For Candida, azoles are preferred. If you’re unsure, use a broad-spectrum azole cream. If it doesn’t improve in 7 days, see a doctor - you might have the wrong diagnosis.
Is fungal skin infection dangerous?
For healthy people, no - it’s just annoying. But for those with weak immune systems, diabetes, or chronic illness, fungal infections can spread deeper, become systemic, and even be life-threatening. Candida auris is a growing concern in hospitals. Don’t ignore persistent rashes if you’re at higher risk.
If you’ve ever felt like your skin infection was "just a rash," think again. Fungal infections are common, treatable - but only if you treat them right. Know the signs. Know the risks. And don’t wait until it spreads.

Comments
Amber Lane
Been there - diaper rash that wouldn’t quit until I switched to zinc oxide + clotrimazole. No more guessing games.
January 21, 2026 AT 05:35
Jerry Rodrigues
Finally someone explains why my athlete’s foot came back after 3 weeks of Lotrimin. I stopped too early. Dumb move.
Now I finish the whole bottle. Even when it looks fine.
January 22, 2026 AT 20:29
Dee Monroe
It’s wild how we treat fungal infections like they’re a personal failure. Like if you just washed better or wore cotton more, you wouldn’t get them. But the truth? Fungi don’t care about your hygiene habits - they care about warmth, moisture, and opportunity. Your immune system is the real gatekeeper. And when it’s tired from stress, sugar, antibiotics, or sleeplessness? The fungi throw a party. We need to stop shaming people and start treating the system, not just the symptom. Probiotics aren’t a fad - they’re ecological restoration. You’re not just killing yeast, you’re rebuilding the neighborhood. And honestly? That’s the most compassionate way to heal.
January 24, 2026 AT 15:21
Sangeeta Isaac
so i had this rash under my boob for months n thought it was eczema lmao
then i saw a derm who was like ‘uhhh this is candida u dum dum’
clotrimazole for 10 days and boom. gone.
why do docs even try to guess anymore??
January 25, 2026 AT 20:06
Malvina Tomja
Of course you’re telling people to use OTC creams. Meanwhile, in the real world, 60% of ‘ringworm’ cases are actually psoriasis misdiagnosed by Google. You’re enabling self-treatment disasters. And don’t even get me started on ‘probiotics for yeast’ - that’s supplement marketing dressed as science. If your immune system is failing, don’t blame your gut flora. Blame your doctor who didn’t check your HbA1c.
January 26, 2026 AT 14:34
Kevin Narvaes
so like… if fungus eats keratin… does that mean my dead skin is basically its buffet?
and if i stop scratching… am i just starvin’ it out?
also why does my cat have ringworm but i don’t? is it karma?
January 27, 2026 AT 23:10
Alex Carletti Gouvea
Why are we letting fungi dictate public health? In my country, we don’t tolerate this kind of weakness. You get infected? Fix it. No excuses. No probiotics. No ‘maybe it’s not eczema.’ Just treat it. Hard. Fast. No whining.
January 28, 2026 AT 15:30
Stephen Rock
Terbinafine is overrated. I’ve seen 3 cases where it made the rash worse. And now you’re telling me to take it for 12 weeks? My liver’s not a lab rat. This whole thing feels like Big Pharma’s way of keeping us on pills forever. They don’t want you cured - they want you compliant.
January 28, 2026 AT 16:47
michelle Brownsea
And yet… you still didn’t mention that Candida auris is being deliberately ignored by the CDC because it’s ‘too expensive’ to track in nursing homes. People are dying in silence - while influencers post ‘yeast cleanse’ videos. This isn’t medicine. It’s capitalism with a stethoscope.
January 29, 2026 AT 02:37
Barbara Mahone
As someone who grew up in a household where fungal infections were treated with neem oil and boiled turmeric water - I’m relieved to see evidence-based guidance. But I also worry. In many communities, seeing a dermatologist is a luxury. We need affordable KOH tests in primary clinics. Not just in urban centers.
January 31, 2026 AT 00:41
Andrew Rinaldi
There’s a quiet dignity in letting your body heal - if you give it the right conditions. Dry skin. Clean clothes. No steroids. Patience. It’s not about being perfect. It’s about being consistent. I used to think antifungals were magic. Now I know they’re just tools. The real cure? How you live.
February 1, 2026 AT 04:19
Samuel Mendoza
Probiotics for yeast? That’s not science. That’s TikTok. If it worked, everyone would be taking it. But 90% of people still get recurring infections. So stop pretending supplements are a fix. Use the meds. Or don’t. But don’t lie to yourself.
February 1, 2026 AT 18:55
MAHENDRA MEGHWAL
Thank you for this comprehensive overview. As a medical professional from India, I encounter these infections daily - often misdiagnosed due to resource constraints. The KOH prep remains underutilized in rural clinics. We need training, not just pamphlets. Your clarity is a gift to those without access to specialists.
February 2, 2026 AT 00:34
Roisin Kelly
So now we’re supposed to believe that ‘Candida auris’ is real? Or is this just another fear-mongering scare tactic? I’ve read that 80% of ‘superbugs’ are inflated by hospital PR. Who benefits from this panic? Pharma? The CDC? The people who sell antifungal sprays on Amazon?
February 3, 2026 AT 08:26
lokesh prasanth
ringworm = not worms. candida = not bacteria. but still people think it’s ‘just dirt’. we need more education. not just meds.
February 4, 2026 AT 05:56