When your immune system turns against your own body, food can become one of your most powerful tools. Autoimmune diseases - like rheumatoid arthritis, Hashimoto’s thyroiditis, Crohn’s disease, and lupus - aren’t just about genetics or bad luck. Growing evidence shows that what you eat directly influences inflammation levels, symptom severity, and even how much medication you might need. This isn’t about miracle cures. It’s about using food as medicine to calm an overactive immune system.
What Does an Anti-Inflammatory Diet Actually Look Like?
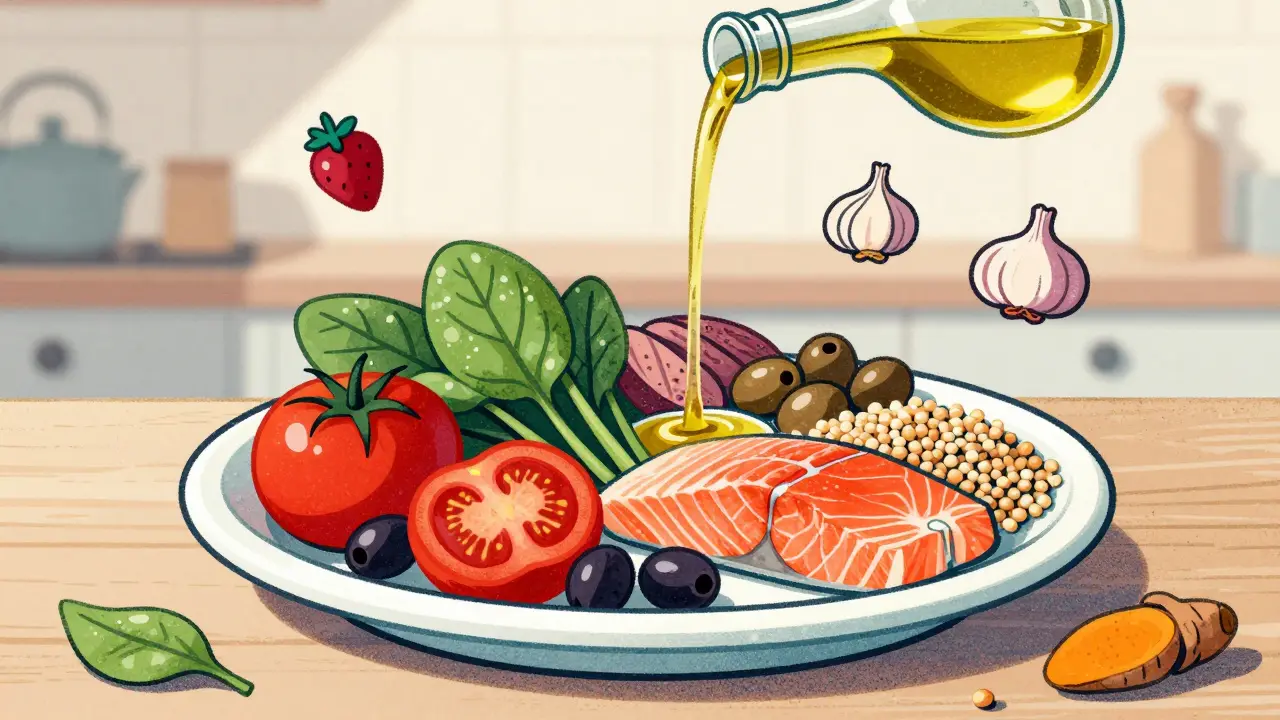
There’s no single "autoimmune diet." Instead, there are several well-researched patterns that share the same goals: reduce inflammation, support gut health, and nourish your cells with real food. The most studied is the Mediterranean diet. It’s not fancy. It’s simple: lots of vegetables, fruits, whole grains, beans, nuts, olive oil, and fatty fish like salmon or sardines. Two tablespoons of extra virgin olive oil a day, three servings of fish weekly, and at least seven servings of plants daily. That’s it. Other patterns include the DASH diet (originally for blood pressure), vegetarian and vegan diets, and the ketogenic diet. Even the Autoimmune Protocol (AIP) diet - which removes common triggers like grains, dairy, eggs, nuts, seeds, nightshades, and coffee for 5-8 weeks - is built on the same foundation: remove the noise, let the body heal, then reintroduce carefully. The key isn’t perfection. It’s consistency. Studies show people who stick with these patterns for at least two years see measurable drops in C-reactive protein (CRP), a key marker of inflammation. One 2022 meta-analysis found CRP levels fell by 20-30% in autoimmune patients following anti-inflammatory diets compared to those eating standard Western meals.What Foods Fight Inflammation?
Not all plants are equal. Some have superpowers when it comes to calming immune responses.- Berries - blueberries, strawberries, raspberries - are packed with anthocyanins, which block inflammatory signals in cells.
- Leafy greens - spinach, kale, Swiss chard - are rich in antioxidants and fiber, feeding good gut bacteria that produce butyrate, a compound linked to 20% lower levels of IL-6, a major inflammatory cytokine.
- Fatty fish - salmon, mackerel, anchovies - provide EPA and DHA, omega-3 fats that reduce pro-inflammatory cytokines by 15-25% at doses of 2-4 grams daily.
- Olive oil - especially extra virgin - contains oleocanthal, a compound that works like ibuprofen to inhibit NF-κB, a master switch for inflammation. In vitro studies show it cuts this pathway by 30-40%.
- Legumes - lentils, chickpeas, black beans - deliver fiber and plant protein. Three servings a week can help stabilize blood sugar and reduce systemic inflammation.
- Spices - turmeric, ginger, garlic - aren’t just flavor. Curcumin in turmeric and gingerols in ginger directly suppress inflammatory pathways.
What Should You Avoid?
The real enemy isn’t just sugar. It’s the entire industrial food system built around processed ingredients.- Added sugars - even one soda a day can spike inflammation. Limit to 25 grams daily - that’s about six teaspoons.
- Refined carbs - white bread, pasta, pastries - break down quickly into sugar, triggering insulin spikes and inflammation.
- Trans fats - found in fried foods and margarine - are directly linked to higher CRP levels and increased autoimmune flare risk.
- Excess saturated fat - especially from processed meats and industrial dairy - can worsen gut permeability and immune activation.
- Processed foods - anything with unpronounceable ingredients, preservatives, or artificial additives - disrupt the gut microbiome, which controls up to 70% of your immune system.

Which Diet Has the Strongest Evidence?
Not all anti-inflammatory diets are created equal when it comes to proof. The Mediterranean diet leads the pack. A 2021 trial with 2,500 rheumatoid arthritis patients showed a 22% drop in disease activity scores and 18% lower CRP compared to standard diets. Adherence was high - 85% stuck with it after six months. Vegetarian and vegan diets also show strong results. A meta-analysis of over 21,000 people found vegetarians had 26% lower CRP levels than omnivores - but only if they’d been on the diet for at least two years. The catch? Vitamin B12 deficiency risk jumps 300% without supplementation. The keto diet is getting attention. A November 2023 study from UCSF showed that when mice produced higher levels of β-hydroxybutyrate (βHB) - the main ketone body - their autoimmune symptoms dropped by 40%. The mechanism? βHB triggered gut bacteria to produce indole lactic acid, which blocked harmful T helper 17 cells linked to MS and other autoimmune conditions. Human trials are still small, but the science is promising. The AIP diet is popular in patient communities. Observational studies report 60-70% of people with Hashimoto’s or IBD feel better after eliminating triggers. But there are no large randomized trials yet. Still, many report real wins: "Eliminating nightshades cut my psoriatic arthritis pain in half," one patient wrote.What Do Real People Experience?
Behind the numbers are real lives. On Reddit’s r/Autoimmune community (125,000 members), a 2022 survey of 1,247 people found 68% felt their symptoms improved with dietary changes. One person wrote: "After three weeks on Mediterranean eating, my morning stiffness went from two hours to 30 minutes." Another said: "My Crohn’s flares dropped from monthly to quarterly." But it’s not easy. Many struggle with social situations. "I can’t eat at restaurants or family dinners without feeling like an outcast," shared one AIP follower. Others report the keto adaptation phase as brutal: "Week one felt like the flu. I couldn’t get out of bed." The Arthritis Foundation found 72% of respondents thought diet helped - but 58% said conflicting advice made it hard to know where to start.How to Start - Without Overwhelming Yourself
You don’t need to overhaul your life overnight. Start small:- Swap one processed snack for a handful of almonds or an apple.
- Add one extra serving of vegetables to lunch or dinner.
- Replace sugary drinks with water, herbal tea, or sparkling water with lemon.
- Use olive oil instead of butter or vegetable oil for cooking.
- Include fatty fish twice a week - canned salmon works fine.

The Bigger Picture
This isn’t just about food. It’s about recognizing that your immune system listens to what you eat. The global anti-inflammatory diet market is projected to hit $22.3 billion by 2027. Fifty million Americans live with autoimmune conditions - and nearly 70% are already trying dietary changes. More doctors are talking about it: 42% of rheumatologists now regularly discuss diet with patients, up from 28% in 2018. The NIH is funding a major 5-year trial called DIETA, which will compare Mediterranean vs. standard diets in 1,000 early rheumatoid arthritis patients. Results come in 2026. Meanwhile, companies are testing personalized diets based on gut microbiome scans - a future where your food plan is tailored to your unique biology. For now, the message is clear: whole, unprocessed foods reduce inflammation. Processed foods fuel it. You can’t control your genes. But you can control your plate. And that matters more than you think.What About Supplements?
Supplements can help - but they’re not replacements for food. Omega-3 fish oil is the most studied. 23% of autoimmune patients use it, and for good reason. Doses of 2-4 grams daily can reduce joint pain and stiffness in RA. Vitamin D is another key player - low levels are linked to higher autoimmune risk. Most experts recommend 2,000-4,000 IU daily, but get your blood tested first. Avoid high-dose antioxidant supplements unless prescribed. Some, like high-dose vitamin C or E, may interfere with immune regulation in autoimmune conditions. Food sources are safer and more effective.Is This for Everyone?
Yes - but with caveats. If you have kidney disease, talk to your doctor before increasing protein or potassium from plant foods. If you have diabetes, monitor blood sugar closely when shifting to lower-carb patterns. Pregnant women should avoid AIP elimination phases. The goal isn’t to follow a rigid list forever. It’s to find what works for your body. Track your symptoms. Notice how you feel after meals. Keep a simple journal: "Ate salmon + greens - no joint pain." "Ate pizza - swollen fingers." Patterns emerge. This isn’t a diet you quit. It’s a way of eating that supports your health long-term. Even small changes add up. You’re not fixing your immune system. You’re giving it the tools to calm down.Can diet really reverse autoimmune disease?
Diet alone doesn’t reverse autoimmune disease, but it can significantly reduce symptoms, lower inflammation markers, and decrease reliance on medication. Many people with rheumatoid arthritis, Hashimoto’s, or IBD report fewer flares, less pain, and more energy. The goal isn’t cure - it’s control.
How long does it take to see results from an anti-inflammatory diet?
Some people feel better in 2-3 weeks - especially with reduced joint pain or bloating. For deeper changes, like lowered CRP or improved gut lining, it takes 8-12 weeks. The longer you stick with it, the more benefits you’ll see. Consistency beats perfection.
Is the AIP diet safe long-term?
The elimination phase of AIP is meant to be temporary - 5 to 8 weeks. Long-term restriction without reintroduction can lead to nutrient deficiencies and unnecessary food fears. The key is systematic reintroduction: add one food at a time, wait 3-7 days, watch for symptoms. Most people can eventually bring back many foods without flare-ups.
Do I need to go keto to help my autoimmune condition?
No. While ketosis shows promise in early research - especially for neurological autoimmune conditions like MS - the Mediterranean and plant-rich diets have far stronger evidence and are easier to maintain. Keto is not required. It’s an option for some, but not the only path.
Why do some people say diet didn’t work for them?
Many factors: they didn’t give it enough time, they didn’t eliminate key triggers like sugar or processed oils, they didn’t address stress or sleep, or they tried a fad diet instead of a proven pattern. Also, some autoimmune conditions respond better than others. RA and IBD show the clearest benefits. Others, like lupus, may respond more subtly.

Comments
dean du plessis
Been eating mostly plants and fish for a year now and my joint pain is way down. Not magic, just consistent. No supplements, no drama. Just real food. Took about 3 months to notice anything but now I don’t even think about it anymore.
December 28, 2025 AT 18:43
Liz Tanner
So many people treat this like a diet to ‘fail’ instead of a way of living that supports your body. The Mediterranean pattern isn’t about restriction-it’s about abundance. More greens, more olive oil, more laughter at the table. That’s the real medicine.
December 28, 2025 AT 20:04
Babe Addict
Let’s be real-the only reason this works is because it’s low-carb by accident. No one’s gonna tell you that keto is the actual answer because Big Pharma hates ketones. βHB suppresses TH17 cells? That’s not nutrition, that’s pharmacology with a side of kale.
December 29, 2025 AT 15:03
Alex Lopez
While I appreciate the data-driven approach, I must respectfully note that the meta-analysis cited in paragraph three lacks adjustment for confounding variables such as socioeconomic status and physical activity levels. Moreover, the 2023 Western diet study used a non-validated food frequency questionnaire, rendering its conclusions statistically suspect. The reduction in CRP is modest at best, and correlation does not imply causation.
Furthermore, the AIP diet’s anecdotal success rate of 60–70% is not generalizable without randomized controlled trials. One must also consider the psychological burden of chronic dietary restriction, which may exacerbate stress-induced inflammation-thereby negating any physiological benefit.
Lastly, the promotion of olive oil as a panacea ignores the fact that its oleocanthal content varies wildly depending on harvest time, storage, and adulteration. Much of the olive oil sold in the U.S. is diluted with soybean oil. You’re not getting 30–40% NF-κB inhibition-you’re getting a fatty salad dressing with a fancy label.
December 30, 2025 AT 13:28
Liz MENDOZA
I love how this post doesn’t shame people for struggling. I tried AIP for 6 weeks and felt like a monster at family dinners. My mom cried because I wouldn’t eat her lasagna. Then I just started swapping one thing at a time-no elimination, no guilt. Now I eat her lasagna… but I also eat a big salad before it. And I sleep better. That’s my win.
December 30, 2025 AT 21:39
John Barron
Look. If you’re not taking 5g of fish oil daily, 5000 IU of D3, and 1000mg of curcumin with piperine, you’re just playing with your immune system. 🤦♂️ The Mediterranean diet is nice for brunch, but if you’re serious about shutting down TH17, you need pharmacologic-grade nutrients. Also, sleep and circadian rhythm are 80% of the battle. You think your kale smoothie matters if you’re scrolling TikTok at 2am? 😴
December 31, 2025 AT 00:56
Paula Alencar
It is profoundly disheartening to witness the widespread commodification of health as a performative lifestyle aesthetic. The very notion that one can ‘heal’ a complex autoimmune condition through dietary manipulation alone is not only scientifically reductive-it is ethically perilous. When patients are led to believe that their suffering is a consequence of insufficient willpower or culinary diligence, we are complicit in the erasure of systemic medical neglect. The NIH’s DIETA trial is a step forward, yes-but it must be accompanied by universal access to registered dietitians, mental health support, and affordable whole foods. Until then, we are not offering medicine. We are offering moral superiority wrapped in quinoa.
January 1, 2026 AT 05:28
Andrew Gurung
Most of you are just following the same low-fat, plant-based dogma that got us here. 🙄 The real answer? Carnivore. No plants. No lectins. No fiber. Just meat, salt, and water. My psoriasis cleared in 3 weeks. My brain fog vanished. The science? It’s all propaganda from Big Veggie. You think your spinach is healing you? It’s just hiding the inflammation until you eat a tomato. 😈
January 1, 2026 AT 13:18
Gerald Tardif
Start with one thing. One. Maybe swap soda for sparkling water. Then next week, add a handful of berries. You don’t need to become a food scientist overnight. Your body isn’t a lab-it’s a home. Treat it like one. Slow, steady, kind. That’s how real change happens.
January 2, 2026 AT 07:36
Satyakki Bhattacharjee
God gave us food to eat and not to worship. You think eating salmon will save you? You forget the soul. The real disease is pride. When you think your plate makes you better than others, you are already sick.
January 4, 2026 AT 05:16
Nikki Thames
I’m sorry, but if you’re not doing the full AIP protocol with strict reintroduction timelines and daily journaling using a validated symptom scale (like the HAQ-DI), you’re not even trying. And if you’re not testing your microbiome with Viome or Zoe before and after? You’re just guessing. You think your ‘one salad a day’ is helping? It’s barely a placebo. You need data. You need accountability. You need a coach. Otherwise, you’re just another person who gave up after three weeks and blamed the diet.
January 5, 2026 AT 05:35
James Bowers
It’s not about the diet. It’s about compliance. The data is clear: adherence to any anti-inflammatory pattern is the strongest predictor of outcome. The specific diet? Secondary. The average person cannot maintain the Mediterranean diet for more than 14 months without reverting to processed foods. Therefore, the entire premise is flawed. We should be focusing on behavioral economics and food deserts, not olive oil.
January 6, 2026 AT 15:52