For millions of patients, standard prescription medications just don't fit. Maybe they can't swallow pills, have severe allergies, or need a dose that doesn't exist on store shelves. That's where compounded medications step in.
What Are Compounded Medications?
compounded medications are custom-prepared pharmaceutical formulations tailored to individual patient requirements. Unlike mass-produced drugs, these are made by pharmacists in specialized pharmacies to address specific health needs. The practice dates back to pharmacy's origins when all prescriptions were hand-mixed. Today, it's a growing field with the market expected to reach $15.8 billion by 2030.
When Do You Need Them?
Compounded medications become necessary when commercial options fall short. Here are common situations:
- Allergies or intolerances: If you're allergic to dyes, gluten, or preservatives in standard pills, a compounding pharmacist can remove those ingredients.
- Unique dosage needs: Need 1.5mg of a drug when only 1mg and 2mg are available? Compounding can create exact doses for precise treatment.
- Alternative delivery methods: Difficulty swallowing pills? A compounded cream, liquid, or suppository can make taking medication easier-especially for children or elderly patients.
- Combining multiple medications: Some patients take five pills daily. Compounding can merge them into one dose to simplify routines.
For example, a child with ADHD might refuse bitter pills. A compounded cherry-flavored liquid increases adherence from 40% to 95% in some cases. Similarly, seniors with digestive issues may benefit from transdermal gels that bypass the stomach entirely.
Benefits and Risks of Custom Formulas
While compounded medications solve real problems, they come with trade-offs. Here's a quick comparison:
| Feature | Compounded Medications | Commercial Medications |
|---|---|---|
| FDA Approval | Not FDA-approved; safety not verified before use | Thoroughly tested and approved by FDA |
| Dosage Flexibility | Customizable (e.g., 1.5mg doses) | Fixed strengths only |
| Allergen-Free Options | Can exclude allergens like gluten or dyes | May contain common allergens |
| Cost | $30-$500 depending on complexity | $10-$50 for generics |
| Insurance Coverage | Often not covered; varies by plan | Usually covered by insurance |
| Quality Control | Varies by pharmacy; PCAB-accredited have higher standards | Strict manufacturing standards enforced |
But risks exist. The 2012 New England Compounding Center outbreak caused 64 deaths due to contaminated steroid injections. This tragedy led to stricter regulations. Today, only about 350 of 7,500 U.S. compounding pharmacies are PCAB-accredited-meaning they meet rigorous safety standards.
How to Get a Compounded Prescription
Getting compounded meds isn't as simple as walking into a regular pharmacy. Here's the process:
- Consult your doctor: They must identify a need that commercial drugs can't meet. Only about 3-5% of patients require compounding.
- Find a qualified compounding pharmacy: Look for PCAB accreditation. This ensures the pharmacy follows strict quality protocols. You can check the Pharmacy Compounding Accreditation Board website.
- Pharmacist consultation: Your pharmacist will review the prescription and discuss formulation options. They might suggest alternatives if the request isn't appropriate.
Remember: federal law requires a valid patient-pharmacist-provider relationship. No pharmacy can compound drugs without a prescription from a licensed provider. Also, 98% of compounded medications require a prescription, according to the National Community Pharmacists Association.
Costs and Insurance Coverage
Compounded medications often cost more than standard drugs. Basic non-sterile compounds range from $30-$100, while sterile compounds (like IV solutions) can hit $200-$500. Compare this to generic drugs which typically cost $10-$50.
Insurance coverage is tricky. Medicare Part D covers only 42% of compounded medication claims, compared to 78% for regular drugs. Private insurers vary widely-some cover them fully, others not at all. Always check with your insurer before filling a compounded prescription.
That said, the value often outweighs the cost. For patients who can't tolerate standard medications, compounded versions prevent hospital visits or lost productivity. A 2022 survey found 82% of patients who needed compounding would recommend it to others with similar needs.

Regulations and Safety Standards
After the 2012 meningitis outbreak, Congress passed the Drug Quality and Security Act in 2013. This created two pathways:
- Section 503A: Traditional compounding pharmacies regulated by state boards. They must follow USP Chapter <795> for non-sterile and <797> for sterile compounds.
- Section 503B: Outsourcing facilities registered with the FDA. They follow current good manufacturing practices (CGMP) and are inspected more frequently.
As of 2023, 65% of U.S. compounding pharmacies operate under 503A, while 350 are FDA-registered 503B facilities. The FDA has issued 12 warning letters in 2022 alone for violations like improper sterilization or mislabeling. This shows regulators are tightening oversight.
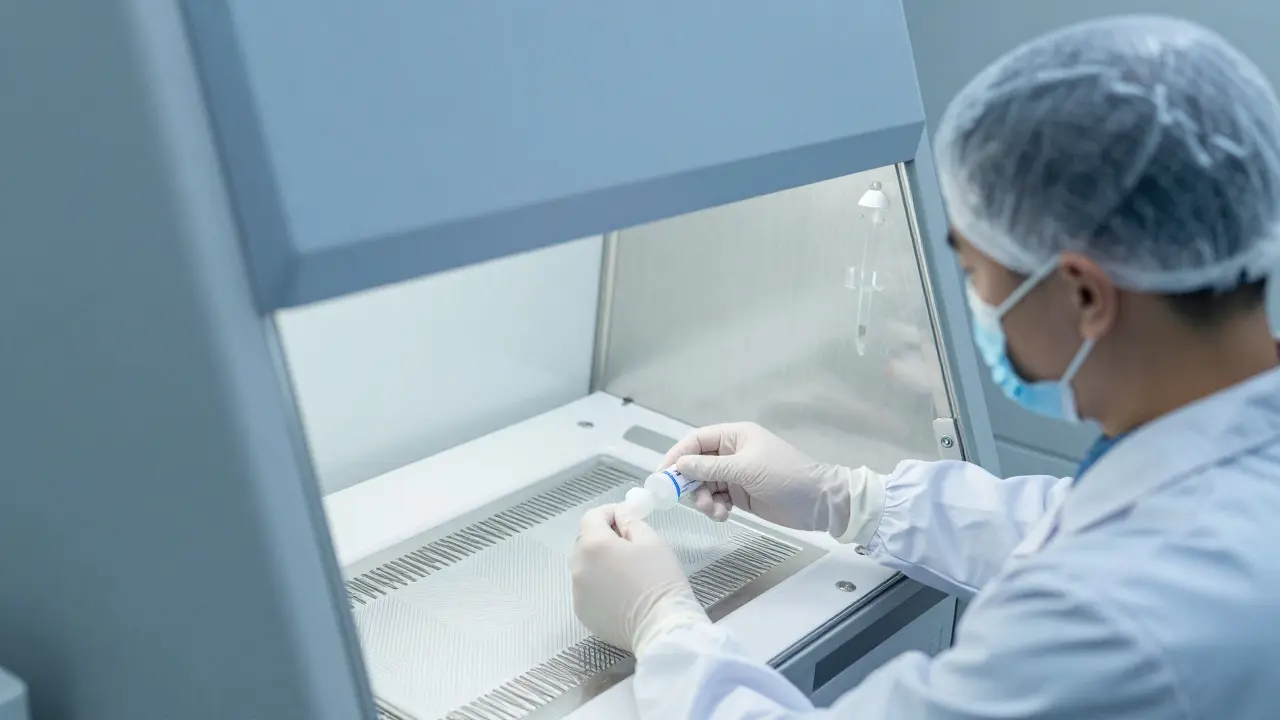
Key standards include environmental monitoring, staff training, and testing for potency and purity. For example, USP Chapter <797> requires sterile compounding to happen in cleanrooms with air filtration systems. These rules help prevent contamination.
Future of Personalized Medicine
Compounding is evolving with advances in science. Some pharmacies now use pharmacogenomic data to tailor medications to a patient's genetic profile. For example, patients with certain CYP2D6 gene variants metabolize drugs differently. Innovation Compounding reports 30% better outcomes in these cases using custom formulas.
However, the FDA remains cautious. Commissioner Califf recently warned against compounding semaglutide for weight loss without proper oversight. The agency stresses that compounded drugs shouldn't replace FDA-approved versions when available.
Experts like Dr. Lucinda Maine of the American Association of Colleges of Pharmacy say the future depends on balancing innovation with safety. "Compounding must preserve its essential role while meeting higher quality standards," she stated in April 2023. With new regulations and technology, this field will likely grow-but only if safety stays central.
Are compounded medications safe?
Safety depends on the pharmacy. PCAB-accredited compounding pharmacies follow strict quality control standards, reducing risks. However, compounded medications aren't FDA-approved, meaning the agency doesn't verify them before use. Always choose a pharmacy with accreditation and ask about their testing procedures. The 2012 NECC outbreak was caused by poor practices, but modern regulations have tightened oversight significantly.
How do I find a reliable compounding pharmacy?
Look for Pharmacy Compounding Accreditation Board (PCAB) accreditation. Only about 350 of the 7,500 U.S. compounding pharmacies have this certification. You can verify accreditation on the PCAB website. Also, check if the pharmacy has state licensing and ask about their quality control processes. Avoid pharmacies that compound in bulk without prescriptions or advertise "ready-made" compounded drugs.
Why aren't compounded medications covered by insurance?
Insurance companies often don't cover compounded medications because they aren't FDA-approved and lack standardized pricing. Each formula is unique, making it hard to set consistent reimbursement rates. Medicare Part D covers only 42% of compounded claims versus 78% for regular drugs. Always contact your insurer before getting a compounded prescription to understand coverage.
Can compounded medications replace FDA-approved drugs?
No. The FDA explicitly states compounded medications should not be used as substitutes for approved drugs when those drugs are available and appropriate. Compounding is meant for situations where commercial options fail-like allergies, unique dosages, or delivery issues. Using compounded versions when FDA-approved alternatives exist poses unnecessary risks.
What's the difference between sterile and non-sterile compounding?
Sterile compounding involves creating medications that enter the bloodstream directly-like IV solutions or eye drops. These require strict cleanroom environments to prevent contamination. Non-sterile compounding makes topical creams, oral liquids, or suppositories that don't enter sterile body areas. USP Chapter <797> governs sterile compounding, while <795> covers non-sterile. Both require rigorous quality controls, but sterile has higher safety thresholds.


Comments
Ariel Edmisten
Great info.
Especially the part about insurance coverage.
Very helpful.
February 8, 2026 AT 09:45
Natasha Bhala
this is reaally helpful
February 9, 2026 AT 15:54
Jesse Lord
I've seen this work for my mom.
She can't swallow pills anymore and the compounded cream has been a lifesaver.
February 11, 2026 AT 08:02
Catherine Wybourne
Ah, compounding-because sometimes the FDA just can't keep up with real human needs.
But let's not forget, 'natural' doesn't always mean better. 💡
February 12, 2026 AT 19:17
Ashley Hutchins
I think this is dangerous.
People should stick to FDA approved meds.
Compounded stuff is risky and unproven.
I know someone who got sick from it. 😠
February 14, 2026 AT 03:55
Niel Amstrong Stein
compounding is cool but also tricky.
Like, it's great for custom needs but gotta be careful with the pharmacy.
🤔 Safety first, folks.
Also, love the stats on 82% recommending it.
Solid.
February 15, 2026 AT 08:21
Paula Sa
It's interesting how compounding fills a gap but also has risks.
Maybe we need better regulations.
Either way, it's good to know options exist.
February 17, 2026 AT 04:07
Mary Carroll Allen
WOW! This is so important.
I had no idea about the 2012 outbreak.
So scary.
But also, the part about pharmacogenomics is mind-blowing.
Can't wait to see where this goes. 💫
February 18, 2026 AT 16:47
Gouris Patnaik
compounding is a western concept.
In India, Ayurveda has been solving health issues for centuries.
Why not use traditional medicine instead?
February 19, 2026 AT 21:39
Lakisha Sarbah
this is really informative.
I had no idea about the PCAB accreditation.
Thanks for sharing!
February 19, 2026 AT 21:44
AMIT JINDAL
compounding is cool but honestly it's a bit overhyped.
I mean, if you have the money, sure, but in India, we have better options like Ayurveda which is way more natural. 🤷♂️
also, the FDA approval thing is just a formality.
real medicine is about results, not paperwork.
plus, most of these compounded drugs are just repackaged stuff. 🤔
the whole system is flawed.
we need to focus on traditional medicine which has been used for thousands of years.
modern science is just catching up.
also, the cost of compounded meds is insane.
why pay so much when Ayurvedic treatments are so affordable? 🤷♂️
furthermore, the quality control in US compounding pharmacies is questionable.
look at the 2012 outbreak.
that's why I think traditional medicine is safer.
also, the environmental impact of pharmaceutical manufacturing is huge.
Ayurveda uses natural ingredients.
plus, the whole idea of compounding is to replace FDA-approved drugs, which is dangerous.
the FDA should crack down on this.
also, many people don't realize the risks.
it's not just about allergies.
it's about contamination.
the 2012 outbreak caused 64 deaths.
that's unacceptable.
so yeah, I think we should stick to traditional medicine. 🤔
February 21, 2026 AT 11:41