Every year, millions of people receive the wrong medication, wrong dose, or wrong instructions from their pharmacy. These aren’t rare mistakes-they’re systemic problems that happen in community pharmacies, hospitals, and even mail-order services. And the consequences? They can be deadly. A 2023 global review found that dispensing errors occur in 1.6% of all prescriptions filled. That might sound small, but with billions of prescriptions written each year, that’s tens of millions of mistakes. In the U.S. alone, medication errors affect around 7 million patients annually. Most of these errors aren’t caused by careless pharmacists. They’re caused by broken systems, rushed workflows, and poorly designed processes.
What Are the Most Common Pharmacy Dispensing Errors?
Not all errors look the same. Some are obvious-like giving someone insulin when they were prescribed metformin. Others are subtle, like giving the wrong strength of a pill or missing a critical drug interaction. According to the Academy of Managed Care Pharmacy and StatPearls, the top five dispensing errors are:- Wrong medication, strength, or form (32% of errors): This includes giving amoxicillin instead of azithromycin, 500mg instead of 250mg, or tablets instead of liquid. It’s the single biggest category.
- Dose miscalculation (28%): Especially dangerous with pediatric, elderly, or kidney-impaired patients. A wrong calculation on warfarin or insulin can lead to hospitalization or death.
- Missed drug interactions or contraindications (24%): Giving a patient an NSAID when they’re on blood thinners, or prescribing an antibiotic they’re allergic to. Antibiotics alone account for 28% of serious error cases, with 41% of those caused by not checking allergies.
- Expired or improperly stored drugs: Medications like insulin, epinephrine, or nitroglycerin degrade quickly if not stored right. Patients get ineffective-or even harmful-doses.
- Wrong duration or route: Giving a 30-day supply when the doctor ordered 7 days, or handing out an IV drug for oral use. One study found that 15% of administration errors involve the wrong route.
Some drugs are far more dangerous when misdispensed. Anticoagulants like warfarin and rivaroxaban are involved in 31% of serious error cases. Opioids, anticonvulsants, and antidepressants are also high-risk. Why? Because small changes in dose or timing can trigger seizures, respiratory failure, or suicidal behavior.
Why Do These Errors Keep Happening?
It’s easy to blame the pharmacist. But the real problem isn’t people-it’s pressure, distractions, and outdated systems.- Workload and time pressure (37% of errors): Pharmacies are understaffed and overworked. One pharmacist told me they’re expected to fill 250+ prescriptions a day. That’s over 30 per hour. When you’re racing from one script to the next, mistakes happen.
- Similar-looking or sound-alike drug names (28%): Lasix and Lopressor. Celebrex and Celexa. Zyrtec and Zoloft. These names look and sound alike. Handwritten prescriptions make it worse. The FDA estimates 22% of verbal prescription errors come from sound-alike names.
- Interruptions (22%): A phone rings. A patient asks a question. A nurse walks in. One study found that if a pharmacist is interrupted three or more times while filling a prescription, the chance of error jumps by 12.7%.
- Illegible handwriting (15-43%): Even in 2025, some doctors still write prescriptions by hand. “Take 1 tab qid” might mean four times a day-or it might be “qid” for “qod” (every other day). Or worse, it’s unreadable.
- Lack of complete patient info: Pharmacists often don’t know about a patient’s kidney function, recent lab results, or other medications they’re taking. Without that, they can’t catch a dangerous interaction.
One hospital pharmacist in Ohio told me: “I’ve caught a wrong dose of morphine because the doctor wrote ‘10 mg’ but the barcode scanned as ‘100 mg.’ The system didn’t flag it because the dose was within the ‘normal’ range. But for a 60-pound child? That’s lethal.”
How to Prevent Dispensing Errors: Proven Strategies
The good news? We know what works. The best prevention isn’t about working harder-it’s about working smarter.1. Double-Check High-Risk Medications
For drugs like insulin, heparin, warfarin, and opioids, a second pharmacist should verify every prescription. One hospital reported a 78% drop in errors after implementing this rule. It doesn’t slow things down-it saves lives.2. Use Barcode Scanning
Barcodes on medication bottles and patient wristbands are now standard in hospitals. When a pharmacist scans the drug, the system checks: Is this the right drug? Right dose? Right patient? Right time? A 2021-2023 survey of 127 hospitals found barcode systems cut dispensing errors by 47.3%. Wrong drug errors dropped by 52%, wrong dose by 49%.3. Implement Tall Man Lettering
This isn’t fancy tech-it’s simple formatting. Write HYDROmorphone instead of hydromorphone, and HYDROxyzine instead of hydroxyzine. The capital letters highlight the difference. Pharmacies that adopted this saw a 56.8% drop in sound-alike errors.4. Use Clinical Decision Support (CDS)
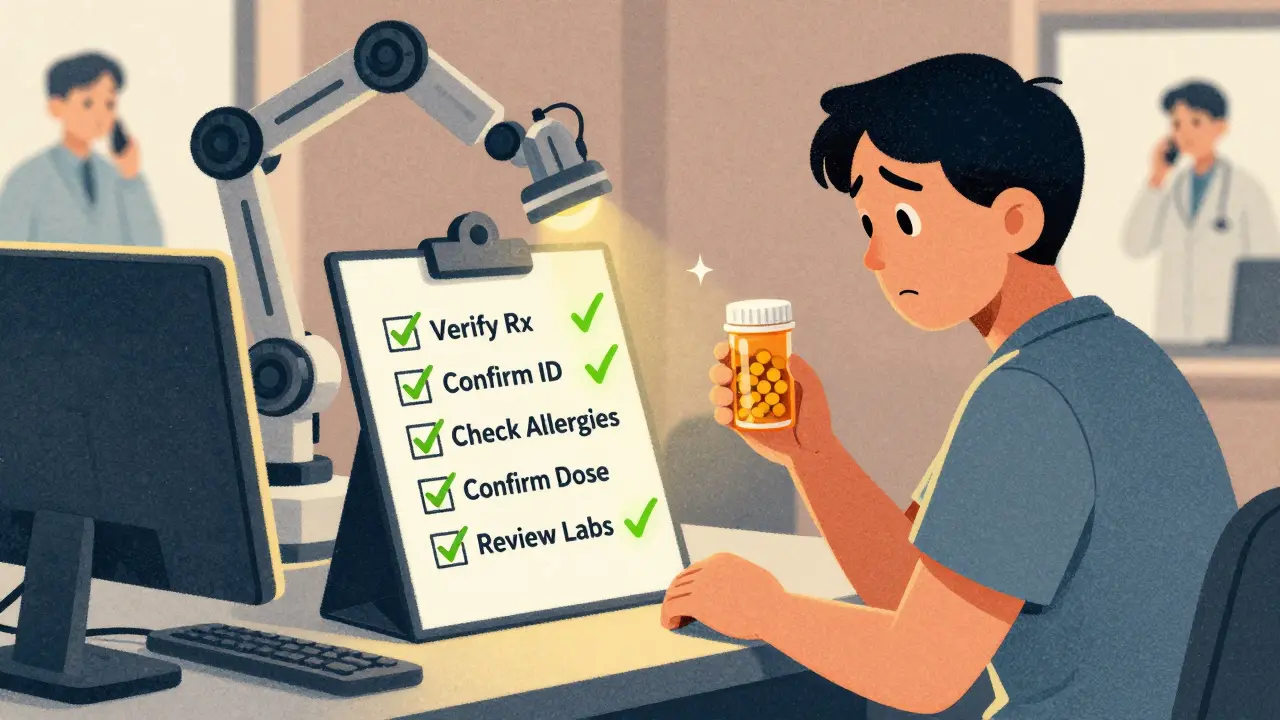
Computer systems that alert pharmacists to allergies, interactions, or incorrect doses are powerful-but only if they’re used right. One study found CDS reduced errors by 43%, but also caused “alert fatigue.” Too many pop-ups, and pharmacists start ignoring them. The fix? Tailor alerts. Only show warnings that matter for the patient’s age, kidney function, and other meds.5. Standardize Processes with Checklists
Just like pilots use checklists before takeoff, pharmacists should use them before handing out medication. A simple five-step checklist:- Verify the prescription against the original order.
- Confirm the patient’s name and date of birth.
- Check for allergies and drug interactions.
- Confirm the correct strength and form.
- Review the patient’s last lab values (e.g., creatinine for kidney drugs).
Pharmacies using this method reduced errors by up to 63% for dose-related mistakes.
6. Improve Communication with Prescribers
When a prescription is unclear, call the doctor. Don’t guess. Many pharmacists avoid calling because they’re afraid of being seen as “inconvenient.” But a 10-second call can prevent a hospital admission.
Technology Isn’t the Whole Answer
Robotic dispensing systems and AI tools are rising. One hospital in Texas installed a robotic system that reduced errors by 63%. But it cost $400,000. And it doesn’t fix everything. AI can miss a patient’s recent change in kidney function. Robots can’t tell if a handwritten note says “take with food” or “take on empty stomach.”Technology helps-but it’s not magic. The best systems combine automation with human judgment. A pharmacist who knows the patient’s history, listens to their concerns, and questions unclear orders is still irreplaceable.
What Patients Can Do to Protect Themselves
You don’t have to rely on the pharmacy to catch every mistake. Here’s what you can do:- Know your meds: Keep a list of everything you take-including doses and why you take them. Bring it to every appointment.
- Ask questions: “Is this the same as what I took last time?” “Why am I taking this?” “What side effects should I watch for?”
- Check the label: Does the name, dose, and instructions match what your doctor told you?
- Report suspicious pills: If the pills look different, smell odd, or come in a strange bottle, ask before taking them.
- Use one pharmacy: If you use multiple pharmacies, they can’t see your full history. One pharmacy has your complete record.
One woman in Manchester told me she caught a wrong dose of levothyroxine because the pill was a different color. She asked, and the pharmacy admitted they’d grabbed the 100mcg instead of the 50mcg. “I didn’t take it,” she said. “I’m glad I asked.”
The Future: What’s Changing?
By 2025, the WHO and ISMP are rolling out a global standard for classifying medication errors. That means pharmacies everywhere will report mistakes the same way-making it easier to learn from them.The FDA is pushing for all pharmacy systems to use the NCC MERP Index by late 2024. That’s a standardized scale that rates errors by how close they came to harming someone. It’s not about punishment-it’s about prevention.
Artificial intelligence is getting better. One AI system tested in 34 hospitals predicted which prescriptions were most likely to be wrong-and flagged them before they were filled. It cut errors by over 50%. But it’s still expensive and not yet common in community pharmacies.
The real win? Shifting from blaming individuals to fixing systems. As Dr. Michael Cohen of ISMP says: “Errors aren’t caused by bad people. They’re caused by bad systems.” When pharmacies stop asking “Who messed up?” and start asking “What broke?”-that’s when real change happens.
Final Thought: Safety Is a Team Sport
Pharmacists, doctors, nurses, patients-we all have a role. No single tool, no matter how advanced, can replace clear communication, careful checks, and a culture that values safety over speed.The goal isn’t zero errors. That’s impossible. The goal is to make errors rare, detectable, and survivable. And that’s something every pharmacy, no matter how big or small, can build.


Comments
Elaine Douglass
My grandma got the wrong blood thinner last year and almost died. I didn't know how common this was until I read this. I'm so glad she asked about the pill color. I'm gonna make sure my whole family keeps a med list now
December 18, 2025 AT 15:15
holly Sinclair
It's fascinating how we've outsourced critical thinking to algorithms and barcodes while ignoring the human element that actually interprets context. The system doesn't know that Mrs. Jenkins has been on warfarin for 12 years and her INR is rock solid-it just sees a number and screams 'alert'. We've created a world where machines do the work but humans bear the blame. Isn't that the definition of institutional cowardice?
December 18, 2025 AT 17:55
Jedidiah Massey
THIS. So important. I work in a pharmacy and we started using the checklist last year. Our error rate dropped like a rock. 🙌 Also, always use one pharmacy-my aunt had a bad interaction because she used three different ones. Don't be lazy, people. Your life matters.
December 20, 2025 AT 07:44
Alex Curran
Australia's been doing barcode scanning and double-checks on high-risk meds since 2018. Errors dropped 50% in 2 years. We still have issues with handwriting but most scripts are e-prescribed now. The real win? Pharmacists actually have time to talk to patients now. It's not magic, just decent resourcing
December 21, 2025 AT 08:11
Allison Pannabekcer
Everyone’s talking about tech fixes but let’s not forget the quiet ones-the pharmacist who takes an extra 30 seconds to read the patient’s history, the nurse who calls the doctor even when they’re busy, the family member who asks ‘why is this pill blue?’ Those small acts are the real safety net. We need to honor them, not just the shiny new systems
December 21, 2025 AT 21:06
Connie Zehner
OMG I knew this was bad but I didn't realize it was THIS bad 😭 I just got my prescription filled and I'm going back to check it right now. I'm so scared. Like… what if I'm one of the 7 million? 😭😭😭
December 23, 2025 AT 09:52
Takeysha Turnquest
They say errors are caused by systems not people but what if the system is just a mirror of our collective apathy? We let pharmacies run like fast-food joints. We don't pay enough. We don't value the work. We treat healing like a transaction. The pills are wrong because we've forgotten how to care
December 24, 2025 AT 19:48
Sarah McQuillan
Yeah but in America we have the best healthcare system in the world. If you're getting the wrong meds it's because you're not paying attention. My cousin works at CVS and they have 10 safety protocols. If you can't handle that, maybe you shouldn't be taking meds
December 25, 2025 AT 10:04
Vicki Belcher
So true about the sound-alike drugs. I once got Zyrtec instead of Zoloft and didn’t notice until I felt like I was floating. I didn’t say anything because I thought it was ‘just me’. Don’t be like me. Ask. Always ask.
December 26, 2025 AT 17:02
Emily P
Has anyone studied how much of this is tied to insurance formularies pushing cheaper alternatives? Like when a pharmacist swaps a brand for generic without telling the patient? That’s not always an error but it can be just as dangerous
December 27, 2025 AT 20:26
Kelly Mulder
It is lamentable that the current paradigm of pharmaceutical dispensing remains so catastrophically under-engineered. The reliance on manual verification, antiquated nomenclature, and human fallibility in high-stress environments is not merely suboptimal-it is an abdication of professional responsibility. One must question the ethical integrity of institutions that prioritize throughput over patient safety. The data are unequivocal.
December 28, 2025 AT 09:18
Jedidiah Massey
^ YES to insurance pushing generics! I've seen patients get switched to a generic that's not bioequivalent and then end up in the ER. Pharmacies get paid more for the cheaper one so they don't tell you. Always ask if it's the same as before!
December 28, 2025 AT 11:20
anthony funes gomez
The systemic failure here is epistemological: we mistake procedural compliance for clinical safety. Barcodes validate labels, not intent. CDS alerts respond to data points, not context. The pharmacist’s tacit knowledge-their intuition honed by years of observing how a patient responds to a dose, how a drug interacts with their lifestyle, how their voice cracks when they say 'I can't afford this'-is the only variable that cannot be algorithmically optimized. And yet, we incentivize speed over silence, volume over vigilance. We are not failing because we lack tools. We are failing because we have forgotten how to listen.
December 28, 2025 AT 22:26