Colorectal Cancer Screening: Why It Starts at 45 Now
Colorectal cancer used to be seen as a disease of older adults. But it’s not anymore. In the last 30 years, the number of people under 50 diagnosed with colon or rectal cancer has risen steadily. By 2025, about 1 in 10 new cases occur in people younger than 50. That’s why major health groups - including the U.S. Preventive Services Task Force and the American Cancer Society - now recommend starting screening at age 45, not 50. If you’re 45 or older, this isn’t optional. It’s one of the most effective ways to avoid a life-threatening diagnosis.
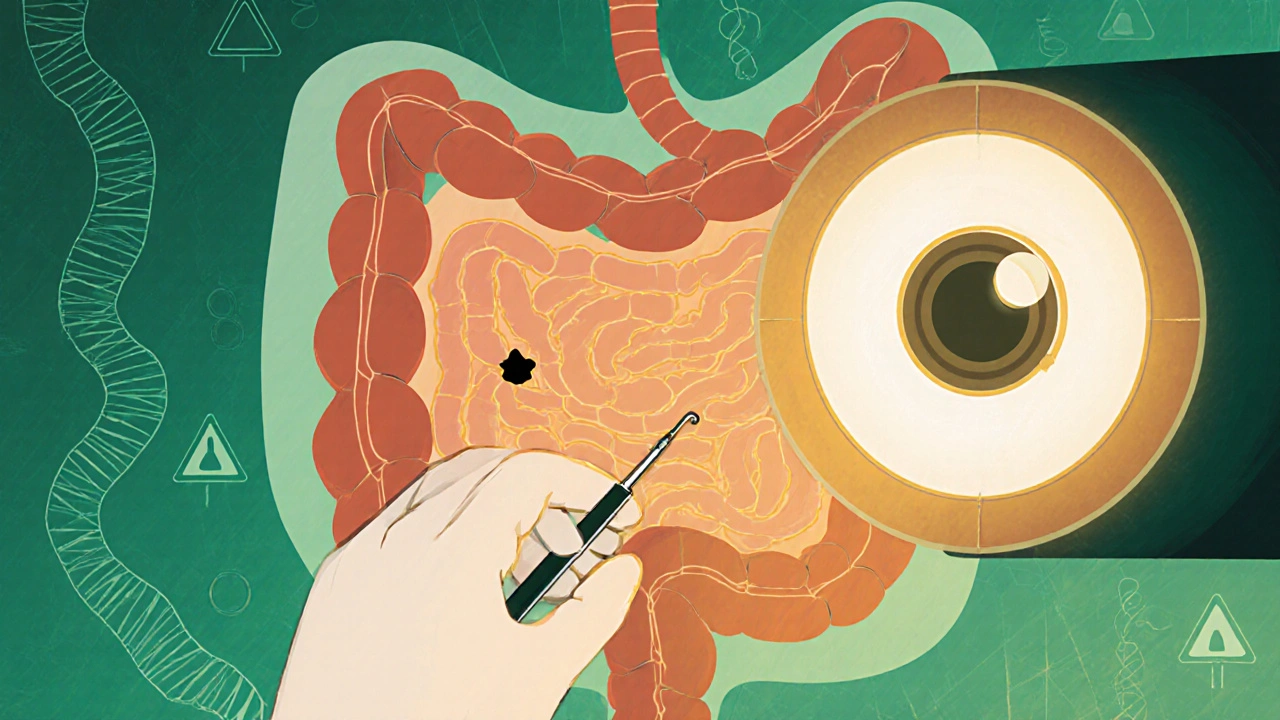
Screening isn’t just about finding cancer. It’s about stopping it before it starts. Most colorectal cancers begin as small, harmless polyps. These can take 10 to 15 years to turn into cancer. A colonoscopy lets doctors spot and remove those polyps right then and there. That’s prevention in action.
How Colonoscopy Works - And Why It’s Still the Gold Standard
Colonoscopy is the most thorough screening tool available. You’ll need to prep your bowels the day before - usually with a strong laxative like polyethylene glycol (PEG). It’s not pleasant, but it’s necessary. On the day of the test, you’ll be sedated. A thin, flexible tube with a camera goes through your rectum and into your colon. The camera shows every inch of your large intestine.
If the doctor sees a polyp, they can remove it during the same procedure. No second visit. No waiting. That’s why colonoscopy reduces your risk of dying from colorectal cancer by up to 65%. Studies show it cuts new cases by 67%. No other test does both detection and prevention in one go.
But it’s not perfect. Complications like bleeding or perforation happen in about 1 out of every 1,000 to 1,500 procedures. That’s rare, but real. Still, for most people, the benefit far outweighs the risk. And if you’re African American, the benefit is even greater - you’re 20% more likely to get colorectal cancer and 40% more likely to die from it than White Americans. Colonoscopy is especially critical for this group.
Other Screening Options - And When They Make Sense
Not everyone wants a colonoscopy. That’s okay. There are other options, each with trade-offs.
- Fecal Immunochemical Test (FIT): You collect a stool sample at home. It checks for hidden blood - a possible sign of cancer or large polyps. It’s simple, cheap, and non-invasive. But you have to do it every year. Sensitivity for cancer is around 80%, but it misses smaller polyps. Adherence is higher than colonoscopy, especially in underserved communities.
- Stool DNA Test (sDNA-FIT): This looks for both blood and abnormal DNA from cancer cells. It’s more sensitive than FIT - detecting 92% of cancers - but it’s also more expensive and gives more false positives. That means more people end up needing a colonoscopy they don’t actually need.
- Flexible Sigmoidoscopy: Only examines the lower third of the colon. Less prep, less sedation. But it misses polyps and cancers in the upper colon. It reduces rectal cancer deaths by 28%, but not overall colon cancer deaths as much as full colonoscopy.
- CT Colonography (Virtual Colonoscopy): Uses X-rays to create 3D images. No sedation, no scope. But you still need bowel prep. And if anything looks abnormal, you still need a colonoscopy to remove polyps. Plus, you’re exposed to low-dose radiation each time.
For people who are healthy and have a life expectancy of more than 10 years, screening should continue through age 75. After 76, it’s a personal decision - based on your health, past screening history, and preferences. If you’ve had clean colonoscopies every 10 years, you might not need more. But if you’ve had polyps before, your doctor may still recommend it.
Who Needs Earlier or More Frequent Screening?
Not everyone follows the 45-year rule. If you’re at higher risk, you may need to start earlier - even in your 20s or 30s.
- Familial Adenomatous Polyposis (FAP): A rare inherited condition that causes hundreds of polyps. Screening often starts at age 10-12.
- Lynch Syndrome: A genetic disorder that greatly increases cancer risk. Colonoscopies every 1-2 years starting at age 20-25.
- Inflammatory Bowel Disease (IBD): If you’ve had ulcerative colitis or Crohn’s for more than 8-10 years, your risk rises. Screening begins at age 45 or 8 years after diagnosis - whichever comes first.
- Family History: If a parent, sibling, or child had colorectal cancer before age 60, or two relatives at any age, you should start screening at age 40 - or 10 years before the youngest case in your family.
For these groups, stool tests aren’t enough. Colonoscopy is the only reliable option. And frequency matters - every 1 to 5 years, depending on your risk level.
Chemotherapy for Colorectal Cancer: What’s Used Today
If screening finds cancer, the next step is treatment. Chemotherapy is often part of that plan - especially if the cancer has spread beyond the colon wall.
There’s no single “best” chemo. It depends on the stage, your overall health, and whether the cancer has specific gene changes.
- 5-FU (Fluorouracil) and Leucovorin: The backbone of colorectal cancer chemo for decades. Still used today, often in combination with other drugs.
- Capecitabine (Xeloda): An oral version of 5-FU. You take pills at home instead of getting IV infusions. Convenient, but can cause hand-foot syndrome - redness, pain, peeling skin.
- Oxaliplatin (Eloxatin): Often combined with 5-FU and leucovorin as FOLFOX. Effective but causes nerve damage in about 70% of patients. Tingling in hands and feet. Can last months or years.
- Irinotecan (Camptosar): Used in FOLFIRI. Can cause severe diarrhea and low blood counts. Often used if FOLFOX stops working.
For advanced cases, targeted drugs are added:
- Bevacizumab (Avastin): Blocks blood vessel growth to starve tumors. Given with chemo.
- Cetuximab (Erbitux) and Panitumumab (Vectibix): Only work if the tumor has a normal RAS gene. If it’s mutated, these drugs won’t help.
Genetic testing of the tumor is now standard. You need to know if your cancer has mutations in KRAS, NRAS, or BRAF. That tells your doctor which drugs will - and won’t - work.
What Happens After Treatment?
Even after surgery and chemo, follow-up is critical. You’ll need regular check-ups every 3 to 6 months for the first few years. Blood tests for CEA (a tumor marker) are common. CT scans or colonoscopies are done yearly or every few years, depending on your risk.
Survival rates vary by stage:
- Stage I: 90%+ 5-year survival
- Stage II: 70-85%
- Stage III: 50-70%
- Stage IV: 14% (if untreated)
Early detection through screening makes all the difference. A 47-year-old man in a 2023 case study had stage I cancer found during his first colonoscopy. His 5-year survival chance? 95%. If it had been found at stage IV, it would’ve been 14%.

Barriers to Screening - And How to Overcome Them
Despite the evidence, only 67% of Americans aged 50-75 are up to date with screening. Among the uninsured, it’s just 58%. Why?
- Prep is awful. Most people say the bowel prep is the worst part. Newer low-volume options are easier, but not always covered.
- Cost and access. Colonoscopy can cost $1,000-$3,000 without insurance. Even with Medicare, you may pay coinsurance. Rural areas have long wait times - sometimes over 60 days.
- Fear and shame. Talking about bowel habits is hard. Many avoid screening because they’re embarrassed.
- Confusion. Too many test options. Patients don’t know which one to pick.
Solutions exist. Automated reminders from your doctor’s office boost adherence by 28%. Patient navigators - real people who help you schedule, prep, and follow up - increase completion rates by 35%. Community health centers using FIT kits see higher participation among Hispanic and Black patients.
What’s Next? Blood Tests and AI
The future of screening is coming fast. Blood tests that detect cancer DNA - like Guardant SHIELD - showed 83% sensitivity in a 2023 trial. They’re not ready for prime time yet, but they could become a first-line option in 5-10 years.
AI is already helping. The GI Genius system, approved by the FDA in 2021, uses artificial intelligence to highlight polyps during colonoscopy. It boosts detection rates by 14%. That means more cancers caught early.
Soon, we may see personalized screening. Instead of everyone getting a colonoscopy at 45, your risk score - based on genetics, diet, lifestyle, and gut bacteria - could determine if you need one at 40, 50, or 60.
Final Thoughts: Don’t Wait Until It’s Too Late
Colorectal cancer is one of the most preventable cancers. You don’t need to be sick to get screened. You don’t need symptoms. You just need to be 45 - or younger if you have risk factors.
Colonoscopy saves lives. Chemotherapy can extend them. But neither works if you don’t act. If you’ve put off your screening, now is the time. Talk to your doctor. Ask about FIT if you’re nervous about colonoscopy. But don’t skip it.
The next time you’re in the waiting room, think of that 47-year-old man. He got screened because his doctor reminded him. He didn’t have symptoms. He didn’t think he was at risk. He’s alive today because he didn’t wait.
At what age should I start colonoscopy screening for colorectal cancer?
For people at average risk, screening should start at age 45. This is the current standard set by the U.S. Preventive Services Task Force, the American Cancer Society, and the American College of Gastroenterology. If you have a family history of colorectal cancer, Lynch syndrome, or inflammatory bowel disease, you may need to start earlier - sometimes as young as 20 or 30. Always talk to your doctor about your personal risk.
Is colonoscopy the best screening method?
Yes, for most people. Colonoscopy is the only test that can both detect and prevent colorectal cancer by removing precancerous polyps during the same procedure. It reduces cancer risk by 67% and death risk by 65%. Other tests like FIT or stool DNA are good alternatives if you can’t or won’t have a colonoscopy, but they don’t prevent cancer - only detect it. If a stool test is positive, you’ll still need a colonoscopy.
What are the most common chemotherapy regimens for colorectal cancer?
The most common chemo combinations are FOLFOX (5-FU, leucovorin, oxaliplatin) and FOLFIRI (5-FU, leucovorin, irinotecan). Capecitabine, an oral drug, is often used as an alternative to 5-FU. For advanced cases, targeted drugs like bevacizumab, cetuximab, or panitumumab are added - but only if your tumor has specific gene markers. Genetic testing of the tumor is required before starting treatment.
Can colorectal cancer be cured if caught early?
Yes. When caught at stage I - meaning the cancer is small and hasn’t spread beyond the colon wall - the 5-year survival rate is over 90%. That’s why screening is so powerful. Most early-stage cancers are removed during colonoscopy or with minor surgery. Chemotherapy is usually not needed at this stage. The key is finding it before it spreads.
Why are African Americans at higher risk for colorectal cancer?
African Americans have a 20% higher incidence of colorectal cancer and a 40% higher death rate than White Americans. The reasons are complex: lower screening rates, later diagnosis, unequal access to care, and possible biological differences in tumor behavior. Colonoscopy is especially important for this group because it’s the most effective way to catch and prevent cancer early. Studies show that when African Americans get screened at the same rate as others, their death rates drop significantly.
What should I do if I’m scared of colonoscopy?
It’s normal to feel anxious. Talk to your doctor. Ask about newer, easier prep options. Many clinics now use split-dose regimens or low-volume solutions that are less harsh. Sedation makes the procedure painless - most people don’t remember it. If you still prefer not to have one, ask about FIT or stool DNA tests. But remember: if those come back positive, you’ll still need a colonoscopy. The best way to avoid a scary diagnosis is to get screened - even if it’s uncomfortable.


Comments
Jennifer Skolney
I got my first colonoscopy at 46 after my mom had polyps removed. The prep was brutal but honestly? The scariest part was waiting for the results. 😅 I’m alive today because I didn’t skip it. If you’re scared, just remember: your future self will thank you.
November 23, 2025 AT 11:30
JD Mette
I’ve been a nurse for 18 years and I’ve seen too many people come in too late. The stats don’t lie. Screening saves lives. It’s not about being scared-it’s about being smart.
November 24, 2025 AT 10:39
Olanrewaju Jeph
In Nigeria, access to colonoscopy is still a luxury. Many patients present with advanced disease due to cost and lack of awareness. I urge all African nations to adopt public screening programs. Early detection is not a privilege-it is a right.
November 25, 2025 AT 01:33
Demi-Louise Brown
The data is clear. Screening at 45 is not optional. It is a medical necessity. Delaying action based on discomfort or fear is not courage-it is negligence.
November 25, 2025 AT 19:53
Matthew Mahar
I did the stool test first because I was terrified of the prep. Got a positive result. Had to do the colonoscopy anyway. The whole thing was over in 20 mins and I napped the whole time. Honestly? The prep was worse than the procedure. I feel like a hero now lol.
November 26, 2025 AT 20:34
Brandy Walley
So now we’re all supposed to be terrified of our own guts because some doctor says so? My grandpa lived to 92 and never had a colonoscopy. He ate bacon every day. Maybe the whole thing is just a big money grab?
November 27, 2025 AT 01:26
shreyas yashas
I’m 43 and my dad had colon cancer at 52. I asked my doc about screening. He said wait till 45. I’m going anyway. Better safe than sorry. Also, the new low-volume prep is way better than the old stuff. No more chugging a gallon of salty water.
November 28, 2025 AT 01:45
Suresh Ramaiyan
There’s a quiet dignity in facing discomfort for the sake of future peace. We fear the unknown, but we rarely fear the consequences of inaction. Screening isn’t about medicine-it’s about responsibility to the life you’re still living.
November 29, 2025 AT 00:21
Katy Bell
I used to make fun of people who did colonoscopies. Then I got a weird cramp. Went in. Found a polyp. They took it out. No big deal. Now I tell everyone. Like, all the time. Seriously, just do it.
November 29, 2025 AT 22:47
Ragini Sharma
sooo i did the stool test and it said positive but i didnt go for colonoscopy cause i was lazy and now i feel bad 😅 maybe next year? lol
November 30, 2025 AT 03:19
Linda Rosie
Evidence-based medicine supports early screening. Compliance improves outcomes. Action is required.
December 1, 2025 AT 06:39
Vivian C Martinez
I know it sounds scary but you’re not alone. My sister was nervous too. She went with her best friend for moral support. They laughed through the prep. Got through it. Both are cancer-free now. You got this.
December 2, 2025 AT 02:02
Ross Ruprecht
I’m 48 and I still haven’t done it. I’ll do it when I’m 50. I’ve got better things to do than sit in a waiting room.
December 3, 2025 AT 01:27
Bryson Carroll
You people act like colonoscopy is some miracle cure. Meanwhile, 70% of people who get chemo still die within 5 years if it’s stage III or IV. And the side effects? Oxaliplatin turns your hands into frozen claws. This whole system is designed to profit off fear, not health.
December 3, 2025 AT 06:41
Lisa Lee
America’s obsession with screening is ridiculous. In Canada we don’t start until 50. Why are you all so desperate to get your colon probed? Maybe you just need to eat less processed food instead of chasing medical tech.
December 3, 2025 AT 08:05