When someone is diagnosed with cancer, chemotherapy is often one of the first treatments mentioned. It’s not new - it’s been saving lives since the 1940s - but that doesn’t mean it’s simple. In fact, chemotherapy is one of the most complex parts of cancer care because it doesn’t just attack cancer. It affects your whole body. And when you’re already taking other medications - for high blood pressure, diabetes, depression, or even heartburn - things get even more complicated. Chemotherapy doesn’t play well with everything. A simple interaction can turn a life-saving treatment into a dangerous one.
How Chemotherapy Actually Works
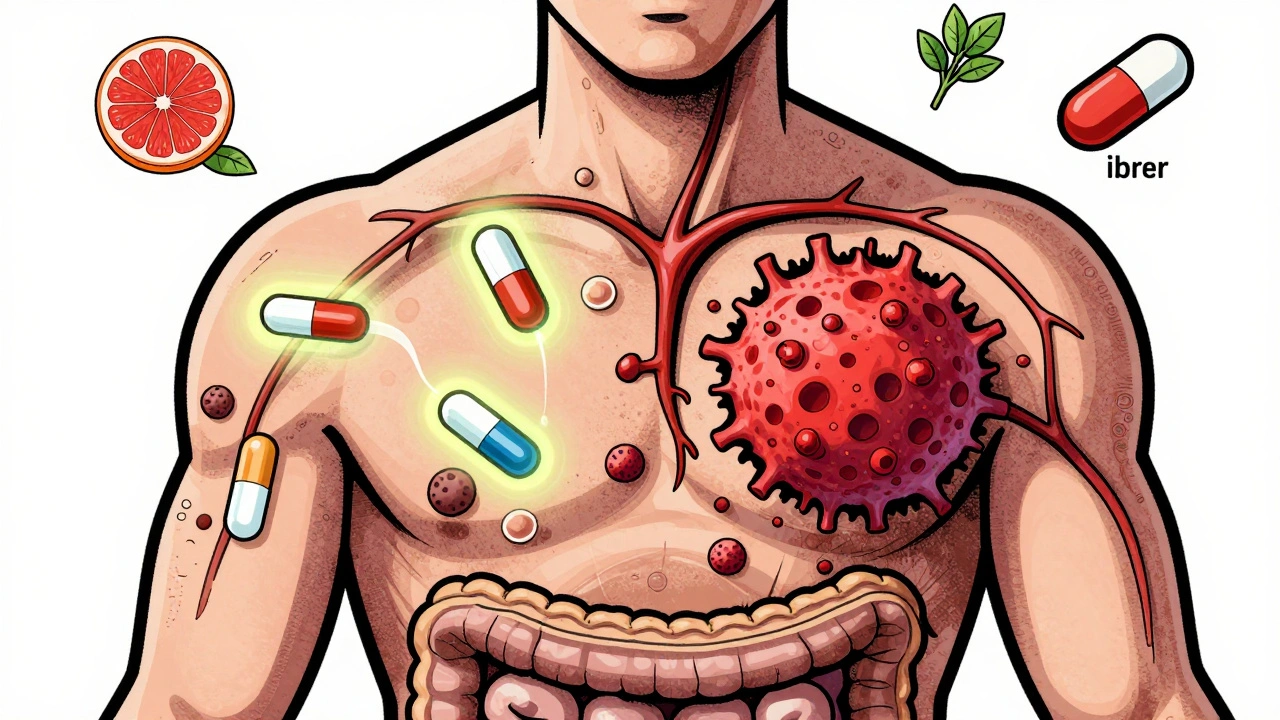
Chemotherapy drugs don’t pick and choose. They target cells that divide quickly. That’s why they hit cancer cells - they grow fast. But they also hit your hair follicles, your gut lining, and your bone marrow. That’s where the side effects come from: hair loss, nausea, low blood counts. There are over 100 different chemotherapy drugs, grouped by how they work. Anthracyclines like doxorubicin damage DNA directly. Alkylating agents like cyclophosphamide mess with cell replication. Antimetabolites like methotrexate trick cells into using fake building blocks so they can’t grow. Each class has its own risks and rules.
Doctors don’t usually give just one drug. Most regimens combine two or three. The BEP combo for testicular cancer - bleomycin, vinblastine, cisplatin - is a classic example. These combinations work because they attack cancer in different ways at the same time. It’s like hitting a moving target from multiple angles. The goal? Kill as many cancer cells as possible before the body can recover. That’s why cycles are spaced out - every 2 to 4 weeks - so your healthy cells get a chance to bounce back.
Why Drug Interactions Are a Big Deal
Here’s the thing: chemotherapy isn’t just a single drug. It’s a system. And that system can be thrown off by something as simple as an over-the-counter painkiller or a herbal supplement. Some drugs make chemotherapy stronger. Others make it weaker. Some increase side effects. Others block the body from breaking down the chemo properly.
Take St. John’s wort, a common supplement for mild depression. It triggers liver enzymes that break down chemo drugs too fast. In one case, a patient on oral cyclophosphamide took St. John’s wort for a few weeks. Their chemo levels dropped by nearly 40%. The cancer didn’t respond. Another example: grapefruit juice. It blocks an enzyme called CYP3A4 that’s responsible for clearing many chemo drugs from the body. The result? Toxic buildup. One study showed grapefruit juice increased levels of docetaxel by over 50% - enough to cause severe nerve damage.
Even common antibiotics can interfere. Azithromycin and clarithromycin can increase the risk of heart rhythm problems when mixed with certain chemo drugs like doxorubicin. And don’t forget about NSAIDs like ibuprofen. They can raise the risk of bleeding, especially when combined with drugs that lower platelet counts. The FDA even requires specific warnings for drugs like pemetrexed - you must take folic acid and vitamin B12, or you risk life-threatening toxicity.
What Patients Are Actually Experiencing
Real people aren’t just statistics. A 2023 survey of over 1,200 chemotherapy patients found that 68% dealt with severe fatigue. Over half still had nausea despite anti-nausea meds. And 41% developed numbness or tingling in their hands and feet - a sign of nerve damage from drugs like paclitaxel. Some of these side effects stick around long after treatment ends.
One woman on a cancer forum described how her hair didn’t just fall out - it came back curly and brittle after taxane chemo. Another shared how her doctor didn’t ask about her daily aspirin for heart health until she had a major bleed during treatment. These aren’t rare. They’re predictable - if you ask the right questions.
And it’s not just physical. About 44% of patients had their treatment delayed because their white blood cell count dropped too low. Black patients faced treatment delays 1.7 times more often than white patients - a gap that points to systemic issues in care access and monitoring.

How Doctors Prevent Dangerous Interactions
Good oncology teams don’t guess. They check. Every single medication - prescription, over-the-counter, supplement, herb - gets reviewed before chemo starts. Board-certified oncology pharmacists verify every regimen. In 98% of U.S. cancer centers, a pharmacist signs off before any chemo is given. That’s not just protocol. It’s survival.
Electronic order systems in major cancer centers now flag potential interactions automatically. If you’re on warfarin and your oncologist tries to order a chemo drug that increases bleeding risk, the system stops and alerts the team. These tools aren’t perfect, but they’ve cut errors by up to 30%.
Some drugs now come with mandatory safety steps. For irinotecan, a common colon cancer drug, doctors test for a gene variant called UGT1A1*28. If you have it, your body can’t process the drug well - you’re at risk for deadly diarrhea. So your dose gets lowered. Same with tamoxifen and CYP2D6 testing. If your body can’t convert it to its active form, the drug won’t work. That’s not guesswork. That’s precision.
What You Can Do to Stay Safe
You don’t need to be a doctor to protect yourself. Here’s what works:
- Keep a complete list of everything you take - including vitamins, CBD, fish oil, melatonin, and herbal teas. Don’t assume it’s "just a supplement."
- Bring that list to every appointment. Don’t wait for the doctor to ask. Say: "I’m on this. Is it safe with chemo?"
- Ask about food and drink. Grapefruit, pomegranate, and even green tea can interfere. Ask what to avoid.
- Don’t start or stop anything without checking. Even if it’s "natural," it can change how your chemo works.
- Know your chemo schedule. If you’re on oral chemo, take it exactly as prescribed. Skipping doses or taking extra because you feel worse can be dangerous.
And if your doctor doesn’t ask about your other meds - speak up. Too many patients assume their oncologist already knows. They don’t. Not unless you tell them.

The Future: Better, Safer Chemotherapy
Chemotherapy isn’t going away. But it’s changing. Newer versions are smarter. Sacituzumab govitecan (Trodelvy) is a chemo drug wrapped in a homing device - it targets only cancer cells that have a specific protein on their surface. That means less damage to healthy tissue. In trials, it cut side effects by nearly half while still shrinking tumors.
Another breakthrough? Using blood tests to see if chemo is working. The ALLIANCE trial showed that checking for leftover cancer DNA in the blood after surgery let doctors stop chemo early in 32% of colon cancer patients - without hurting survival. That’s huge. Fewer cycles. Less toxicity. Better quality of life.
Nanoparticles are coming too. These tiny carriers deliver chemo straight to tumors, avoiding healthy organs. Early results show they could cut systemic exposure by 50-70%. Imagine getting the same cancer-killing power without the nausea, fatigue, or nerve damage.
Bottom Line: Chemotherapy Still Matters
Yes, immunotherapy and targeted drugs are growing. But chemotherapy still cures more people than any other treatment for many cancers. For breast cancer, stage II-III patients on anthracycline-taxane chemo cut their risk of recurrence by 30-40%. For lymphoma and leukemia, it’s often the only thing that works fast enough.
The key isn’t avoiding chemo. It’s using it safely. That means knowing what you’re taking, asking questions, and making sure your whole care team is on the same page. A drug interaction isn’t just a footnote in a medical journal. It’s a real risk - one that can change your outcome. But with the right information and communication, you can avoid it.
Chemotherapy is powerful. But it’s not magic. It’s medicine. And like all medicine, it works best when you’re fully informed.
Can I take over-the-counter painkillers while on chemotherapy?
It depends. Some painkillers like acetaminophen (Tylenol) are usually safe. But NSAIDs like ibuprofen or naproxen can increase bleeding risk, especially if your platelet count is low. Always check with your oncology team before taking anything - even something you’ve used for years.
Do herbal supplements interfere with chemotherapy?
Yes, many do. St. John’s wort, echinacea, ginseng, and milk thistle can all change how your body processes chemo drugs. Some make them less effective. Others make them more toxic. There’s no safe herbal supplement unless your oncologist says it’s okay.
Why do I need to take folic acid and B12 with some chemo drugs?
Drugs like pemetrexed block a key enzyme needed for cell growth - but they also affect healthy cells. Folic acid and vitamin B12 help protect your normal cells from damage. Skipping them can lead to severe side effects like low blood counts, mouth sores, or even life-threatening infections. It’s not optional - it’s part of the treatment.
Can grapefruit juice really affect chemotherapy?
Absolutely. Grapefruit juice blocks an enzyme in your liver that breaks down many chemo drugs. That means the drug stays in your body longer and at higher levels - which can cause serious toxicity. Even one glass can affect drug levels for days. Avoid it completely during treatment unless your doctor says otherwise.
What should I do if I miss a dose of oral chemotherapy?
Don’t double up. Call your oncology team right away. Missing a dose can reduce effectiveness. Taking extra can be dangerous. Each drug has different rules. Your team will tell you whether to skip the dose, take it late, or adjust the next one.
Is chemotherapy still worth it if I have so many side effects?
For many people, yes. Even with fatigue, nausea, or nerve pain, chemotherapy has helped patients live longer and feel better. One study showed that patients who got supportive care along with chemo had 35% higher quality of life. Talk to your team about managing side effects - there are better options now than ever before.
How do I know if my chemo is working?
Your team will monitor you with scans, blood tests, and sometimes tumor DNA tests in the blood. Some patients feel worse before they feel better. Don’t judge effectiveness by how you feel alone. Trust the data your doctors collect - and ask for updates at every visit.
Chemotherapy is hard. But it’s also one of the most powerful tools we have against cancer. The difference between success and danger often comes down to one thing: communication. Know what you’re taking. Tell your team everything. Ask the hard questions. Your life depends on it.

Comments
Casey Mellish
Just got back from my third cycle, and I can’t believe how much I didn’t know about interactions. I was taking melatonin for sleep and fish oil for my joints-never thought either could mess with chemo. My pharmacist flagged them both. Turns out fish oil thins the blood too much with my regimen. Lesson learned: nothing’s ‘just a supplement.’
December 13, 2025 AT 01:40
Tyrone Marshall
There’s something deeply human about how we treat chemotherapy like a magic bullet when it’s really just a very blunt instrument. We’re asking our bodies to survive an internal war-and then we wonder why they break down. The real breakthrough isn’t in the drugs themselves, but in the humility to ask: ‘What else am I taking?’ That’s where healing begins.
December 14, 2025 AT 16:46
Emily Haworth
⚠️ BIG RED FLAG: Did you know Big Pharma doesn’t want you to know grapefruit juice kills chemo? They profit more when you’re sick longer. 🍊💀 They even hide the warnings in tiny print. I found this out after my cousin died. Don’t trust your oncologist-they’re paid by the system. Google ‘chemo suppression industry’.
December 15, 2025 AT 08:32
Tom Zerkoff
It is imperative to emphasize that the pharmacokinetic interactions between chemotherapeutic agents and concomitant medications are not merely theoretical-they are clinically significant and potentially life-altering. The CYP450 enzyme system, particularly CYP3A4 and CYP2D6, plays a pivotal role in the metabolism of numerous oncologic agents. Failure to account for substrate inhibition or induction may result in subtherapeutic exposure or toxic accumulation. Therefore, a comprehensive medication reconciliation, ideally facilitated by a board-certified oncology pharmacist, constitutes a non-negotiable standard of care.
December 15, 2025 AT 16:36
kevin moranga
Man, I wish I’d read this two months ago. I was popping ibuprofen like candy because my joints ached from the chemo fatigue. Didn’t think twice. Then I started bleeding from my gums-scary stuff. My nurse practically yelled at me when I mentioned it. Now I use Tylenol, no more NSAIDs, and I keep a little notebook with everything I take-even the turmeric capsules my wife swears by. Seriously, if you’re on chemo, treat every pill like it’s a grenade. Pull the pin before you swallow.
December 16, 2025 AT 05:51
Alvin Montanez
People think they’re smart because they read a blog or watch YouTube videos and now they think they know more than their oncologist. St. John’s wort? Herbal tea? ‘Natural’ doesn’t mean safe-it means unregulated, untested, and potentially deadly. If you’re going to risk your life because you believe in ‘holistic healing,’ don’t blame the system when you die. This isn’t a wellness retreat. It’s cancer. And it doesn’t care if your supplement is organic.
December 18, 2025 AT 01:54
Lara Tobin
I just want to say thank you to the nurses who remember to ask about your vitamins. I cried when mine did. I’d forgotten I was taking ginger tea for nausea. She caught it. I didn’t even realize it could interfere. You’re not just treating the disease-you’re seeing the person behind the chart. ❤️
December 18, 2025 AT 04:58
Jamie Clark
Chemotherapy is not medicine. It’s chemical warfare. And the fact that we call it ‘treatment’ is a lie we tell ourselves to feel better. They don’t cure you-they poison you slowly until the cancer dies or you do. The real question isn’t ‘how to avoid interactions’-it’s ‘why are we still using this medieval tool in the 21st century?’
December 19, 2025 AT 20:33
Keasha Trawick
Okay, so picture this: your liver is a bouncer at a club. Chemo’s the VIP guest. Grapefruit juice? That’s the guy who slips the bouncer a wad of cash to let everyone in. Suddenly, your chemo’s crashing the party with 10 extra guests-no ID, no rules, just chaos. That’s CYP3A4 inhibition, baby. And now your nerves are screaming, your blood’s thick as molasses, and your oncologist’s face is the color of a stop sign. Don’t be that guy. Skip the juice. Your body’s already fighting a war. Don’t hand the enemy a grenade.
December 21, 2025 AT 16:44
Webster Bull
just say no to grapefruit. and tell your doc everything. even the gummy vitamins. i did. saved my life. 🙏
December 22, 2025 AT 16:47
Deborah Andrich
It’s funny how we treat cancer like a villain to be defeated, but we forget we’re the ones holding the weapon. Chemotherapy doesn’t care if you’re brave or scared, rich or poor-it just does what it does. The real power isn’t in the drugs. It’s in showing up. Writing down every pill. Asking the dumb questions. Showing your list. Being the one who won’t let anyone ignore the details. That’s how you win. Not by being strong. By being stubbornly, annoyingly, beautifully thorough.
December 24, 2025 AT 01:02