When a child isn’t growing like they should-staying small for their age, losing weight, or seeming tired all the time-parents often blame poor eating habits or picky phases. But sometimes, the real culprit is something hidden in plain sight: celiac disease. This autoimmune disorder doesn’t just cause stomach upset. It silently steals nutrients needed for growth, bone development, and energy. The good news? With the right testing and a strict gluten-free diet, most children catch up completely. The challenge? Getting there without missing the signs or slipping up on the diet.
Why Growth Problems Are a Red Flag
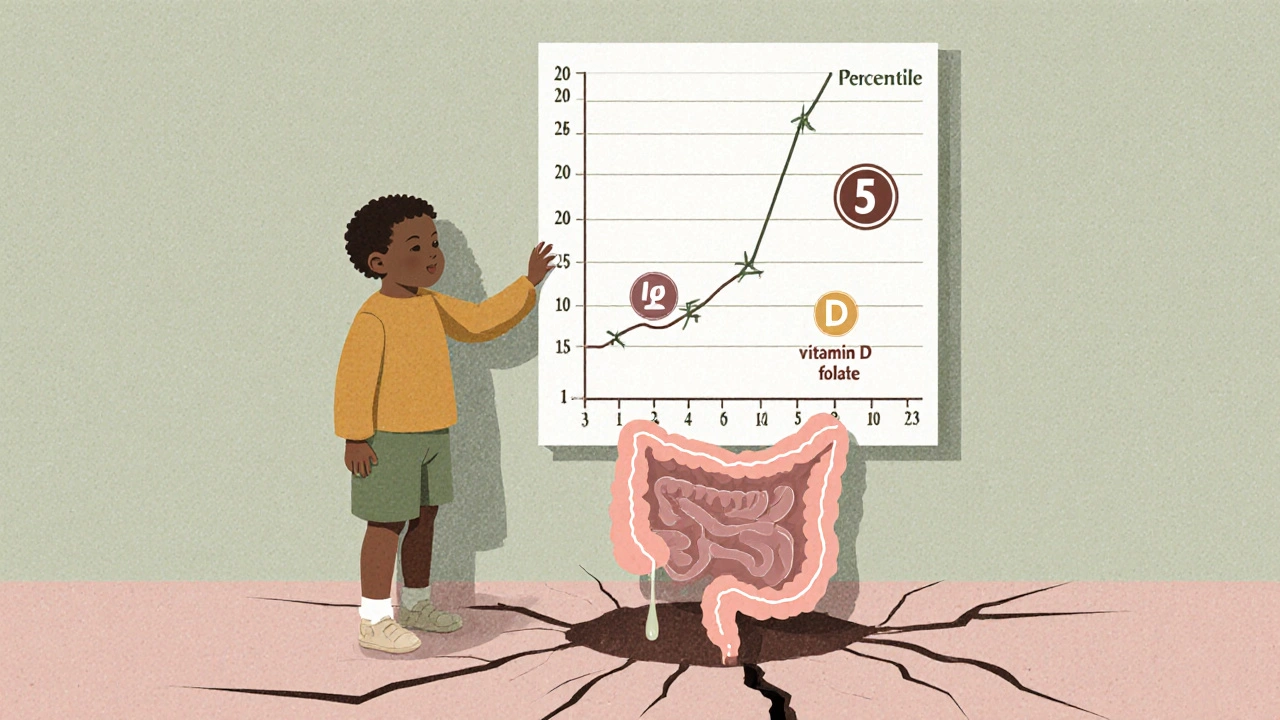
In kids, celiac disease often shows up differently than in adults. Instead of diarrhea or bloating, the first clue might be that they’re not gaining height. A child who’s been stuck at the 15th percentile for years, suddenly falling to the 5th, is sending a signal. So is a child who’s short but has delayed bone age-meaning their skeleton is younger than their calendar age. That’s not just slow growth. It’s a sign the body is starving for nutrients because the gut lining is damaged. Studies show that up to 40% of children brought in for short stature end up being diagnosed with celiac disease. And when they start a gluten-free diet, the body doesn’t just heal-it fights back. Weight usually improves in 6 months. Height? That takes longer. Most kids gain 2 to 4 centimeters per year above their expected rate in the first year. By age 10, 85% reach their target height. But only if the diet is strict.How Doctors Test for Celiac Disease
Testing has gotten smarter. The first step is a simple blood test for tTG-IgA antibodies. This test is accurate in 98% of cases when the child is still eating gluten. But it’s not foolproof. About 2-3% of kids with celiac are IgA deficient, so doctors also check total IgA levels. If the tTG-IgA is more than 10 times the upper limit of normal, and the child has symptoms and carries the HLA-DQ2 or DQ8 gene (which 95% of celiac patients do), a biopsy may not even be needed. That’s a big change from just a few years ago. When a biopsy is done, the damage is clear: flattened villi in the small intestine. These tiny finger-like projections are the body’s nutrient-absorbing tools. In active celiac disease, they’re reduced by up to 90%. That’s why iron, vitamin D, and folate levels crash. Iron deficiency affects nearly half of newly diagnosed kids. Vitamin D levels are low in 40-60%. These aren’t random deficiencies-they’re direct results of a gut that can’t absorb. Bone age X-rays help predict recovery. If a child’s bones are delayed by 1.5 to 2.5 years, their chances of full catch-up growth are over 95%. If bone age is normal, the outlook is less certain. That’s why doctors don’t just look at height-they look at the whole picture.The Gluten-Free Diet: More Than Just Bread
The only treatment for celiac disease is a lifelong gluten-free diet. That means no wheat, barley, rye, or anything made from them. But it’s not just about bread. Gluten hides in soy sauce, malt flavoring, processed meats, and even some vitamins. Cross-contamination is a huge issue. A toaster used for regular bread, a shared knife, or even flour dust in the air can trigger symptoms. Families need to learn how to read labels. The international standard is 20 parts per million (ppm) of gluten-enough to harm a child with celiac. Only 15-20% of regular grocery items are naturally gluten-free. The rest require careful checking. And gluten-free products cost 156-242% more than regular ones, according to Consumer Reports. That’s a financial strain many families didn’t expect.
Tracking Progress: Numbers That Matter
Adherence isn’t just about willpower-it’s about tracking. Every 6 to 12 months, doctors check tTG-IgA levels again. Normal levels mean the gut is healing. Persistent high levels? That’s a warning sign. About 20-30% of kids still test positive even when parents think they’re doing everything right. Often, it’s hidden gluten. Growth is the best real-time indicator. Infants should gain 15-30 grams per day. Older kids should show a height velocity jump of 2-4 cm per year above their predicted rate. If that doesn’t happen, it’s time to dig deeper. Is the child eating out too much? Are school lunches safe? Is there another condition-like thyroid disease or growth hormone deficiency-interfering?Why Adherence Falls Apart-And How to Fix It
Adherence drops sharply in adolescence. Teens want to fit in. Birthday cakes, pizza parties, school trips-they feel left out. One 14-year-old shared that skipping the diet led to daily stomach pain and missed school. Another parent said their 7-year-old gained 2.3 kg in three months but took 14 months to start growing taller again. Schools are a major risk. A 2022 study found 58% of kids with celiac had gluten exposure at school. That’s why a 504 plan is critical. It legally requires the school to provide safe meals, clean prep areas, and staff training. Without it, kids are on their own. Support groups help. Families connected to local celiac chapters report 25-30% better adherence. Knowing other parents who’ve been there makes a difference. So does seeing results. One family saw their child’s height standard deviation score improve from -2.1 to -0.3 in 18 months. That’s not just growth-it’s a life changed.
What Happens If You Don’t Stick to the Diet
Skipping the gluten-free diet isn’t just about discomfort. Long-term, it raises the risk of serious problems. Persistent inflammation increases the chance of lymphoma by 2-3 times, according to Swedish population data. Bone density stays low. Puberty can be delayed. Fertility issues can show up later in life. And not every child catches up fully. About 5-10% of kids, even with perfect diet adherence, don’t reach their genetic height potential. That’s when doctors look for other causes-growth hormone deficiency, thyroid problems, or even undiagnosed food intolerances.What’s on the Horizon
There’s no cure yet, but research is moving. Drugs like larazotide acetate, designed to block gluten from triggering the immune response, are in late-stage trials. They won’t replace the diet-but they might make accidental exposure less dangerous. Immunotherapy trials, like Nexvax2, have stalled, but the science is still evolving. The most powerful tool remains the gluten-free diet. And the most important message? Start early. Kids diagnosed before age 5 have a 98% chance of reaching their full height. After age 10, that drops to 85%. Every month counts.Can a child outgrow celiac disease?
No. Celiac disease is a lifelong autoimmune condition. The body never stops reacting to gluten. A gluten-free diet manages the disease but doesn’t cure it. Stopping the diet-even for a short time-will cause intestinal damage to return.
Is a gluten-free diet healthy for a child without celiac disease?
Not necessarily. Gluten-free processed foods are often lower in fiber, iron, and B vitamins, and higher in sugar and fat. Unless a child has celiac disease, a diagnosed wheat allergy, or non-celiac gluten sensitivity, there’s no proven health benefit to avoiding gluten. In fact, unnecessarily restricting grains can lead to nutritional gaps in growing children.
How long does it take for a child to feel better after starting a gluten-free diet?
Symptoms like diarrhea, bloating, and fatigue often improve within days to weeks. Energy levels can bounce back in as little as 10-14 days. But gut healing takes longer. Blood tests usually normalize in 6-12 months. Height catch-up can take 18-24 months, especially in older children.
Should siblings of a child with celiac disease be tested?
Yes. First-degree relatives have a 5-10% chance of developing celiac disease, even without symptoms. The American Academy of Pediatrics recommends screening siblings every 2-3 years, or sooner if symptoms appear. Testing should include tTG-IgA and total IgA, with HLA gene testing if results are unclear.
Can a child with celiac disease eat oats?
Pure, uncontaminated oats are generally safe for most children with celiac disease after the gut has healed. But most commercial oats are processed in facilities that also handle wheat, barley, or rye. Only oats labeled “gluten-free” and certified by a trusted program should be used. Start with small amounts and monitor for symptoms.
What should parents do if their child keeps testing positive for tTG-IgA despite a gluten-free diet?
First, rule out hidden gluten sources: shared kitchen tools, cross-contamination at school, medications, or cosmetics. Keep a detailed food and symptom log. Consider consulting a registered dietitian specializing in celiac disease. If gluten exposure is ruled out, evaluate for other conditions like refractory celiac disease, thyroid dysfunction, or growth hormone deficiency.
Is there a vaccine or pill to treat celiac disease?
No. As of 2025, the only proven treatment is a strict, lifelong gluten-free diet. Several drugs are in clinical trials, like larazotide acetate, which helps reduce symptoms from accidental gluten exposure. But none replace the diet. Any product claiming to cure or neutralize gluten should be viewed with caution.

Comments
Gordon Mcdonough
This post is literally life-saving info but nobody talks about how the gluten-free aisle is a scam? $12 for a single gluten-free bun? My kid’s diet costs more than our rent. And don’t get me started on school lunches-teachers don’t even know what gluten is. They think it’s a trend. It’s not. It’s a death sentence if you slip up.
November 17, 2025 AT 09:04
satya pradeep
I’m a pediatrician in Mumbai and we see this ALL the time. Kids with stunted growth, iron deficiency, and no one thinks of celiac. We test tTG-IgA first, always. But here’s the problem-most parents think it’s ‘just a stomach bug’ or ‘bad food’. By the time they come, the villi are already flattened. Early detection = full recovery. Don’t wait for diarrhea. Wait for growth failure.
November 19, 2025 AT 07:04
Prem Hungry
I’ve been helping families manage celiac for 12 years. The key is not just diet-it’s mindset. Start with simple swaps: rice, potatoes, eggs, chicken. No need to buy expensive gluten-free pasta right away. And always, ALWAYS check vitamins-many have hidden gluten. I had a mom cry because her 8-year-old was still losing weight… turns out the ‘gluten-free’ gummy vitamins had barley malt. Simple fix. Big difference.
November 19, 2025 AT 10:19
Leslie Douglas-Churchwell
Let’s be real. Big Pharma and the wheat industry are suppressing celiac research. Why? Because if everyone knew how widespread this is, gluten-free products would become regulated like insulin. And then they’d lose billions. The ‘20ppm’ standard? That’s a joke. Studies show even 5ppm can trigger autoimmunity in sensitive kids. And don’t get me started on glyphosate in wheat-linked to gut permeability. This isn’t medicine. It’s corporate control.
November 19, 2025 AT 19:22
shubham seth
Celiac isn’t a disease-it’s a betrayal. Your own body turns on you because of a protein that’s been in human diets for 10,000 years. And now we’re supposed to believe a 14-year-old can survive without pizza? That’s not diet. That’s emotional torture. The only thing worse than the disease is the guilt. And the cost. And the judgment. ‘Why can’t you just eat a slice?’ Like I’d willingly ruin my kid’s pancreas.
November 20, 2025 AT 07:53
Kathryn Ware
I just want to say how much this post helped me. My daughter was diagnosed at 6, and we were drowning in confusion. The part about bone age X-rays? That was a game-changer. We found out hers was delayed by 2 years-so we knew she’d catch up. And the 504 plan? We got it within 3 weeks. Now she eats lunch with her friends, no shame. I joined a local group and we do monthly gluten-free potlucks. It’s not perfect, but it’s healing. 💕
November 21, 2025 AT 04:34
kora ortiz
If your child isn’t growing, test for celiac. No excuses. No waiting. No ‘maybe it’s just a phase’. This isn’t optional. It’s survival. The stats don’t lie: 85% reach target height if diagnosed early. That’s not hope. That’s science. And if your school won’t accommodate? File a complaint. Your kid’s future is worth more than their lunch tray. Stop being polite. Be relentless.
November 22, 2025 AT 16:44
Jeremy Hernandez
Look, I get it. You’re scared. But let’s cut the drama. Gluten-free diets are a fad for neurotic moms. Most kids who are ‘short’ just have bad genes. My cousin’s kid was diagnosed with celiac at 4. He’s 17 now and still 5’2”. No magic diet fixes height. And those ‘gluten-free’ products? Full of sugar and carbs. You’re trading one problem for another. Stop the fear-mongering.
November 24, 2025 AT 09:02
Tarryne Rolle
Is celiac disease just modern anxiety made physical? We’ve pathologized a biological response to an agricultural staple that evolved with civilization. Why do we assume the body must adapt to the diet, and not the diet to the body? The real tragedy isn’t gluten-it’s the loss of trust in our own biology. We’ve outsourced health to labels, tests, and corporate-approved foods. The child doesn’t need a diet. They need a reconnection.
November 25, 2025 AT 08:52
Kyle Swatt
I’ve watched my nephew go from barely talking at age 5 to acing science fairs at 11 after going gluten-free. The change wasn’t just physical-it was emotional. He stopped zoning out. Started laughing. Made friends. This isn’t just about villi or antibodies. It’s about a child finally feeling like themselves. The diet isn’t a punishment. It’s a permission slip to live. And yeah, it’s expensive. And annoying. But it’s not the enemy. The enemy is ignoring the signs.
November 26, 2025 AT 06:17
Deb McLachlin
I appreciate the thoroughness of this post. However, I must note that the prevalence of celiac disease in South Asian populations is significantly underreported due to genetic heterogeneity and limited screening infrastructure. The HLA-DQ2/DQ8 association is less dominant in Indian cohorts, where DQ7 and other variants may play a role. This suggests that reliance on Western diagnostic criteria may lead to underdiagnosis in non-European populations. Further research is warranted.
November 27, 2025 AT 05:56
saurabh lamba
So we’re spending thousands on gluten-free food… but the real issue is the soil. Glyphosate. GMO wheat. Corporate monoculture. This isn’t a medical issue. It’s an ecological collapse. We’re treating symptoms while the planet burns. And no one’s talking about it. Just give the kid more vitamins and call it a day. Pathetic.
November 27, 2025 AT 22:12
Kiran Mandavkar
The entire narrative here is colonial. Gluten-free diets are a Western luxury. In India, we’ve eaten wheat for millennia without this hysteria. Why do we pathologize a natural biological variation? Maybe the child is just malnourished from poverty, not gluten. Or maybe their gut flora is broken from antibiotics. Let’s stop blaming the grain and start blaming the system.
November 28, 2025 AT 07:48
Eric Healy
I’m the author. Just wanted to say thank you to everyone who shared their stories. The comment about school lunches? That’s why I wrote this. We need to stop pretending this is a choice. It’s medical. And the silence is killing kids. If you’re reading this and your child’s growth has stalled-get tested. Don’t wait. You’re not overreacting. You’re saving them.
November 29, 2025 AT 05:18