Getting diagnosed with depression is only the first step. What matters more is knowing which kind of depression you have. Bipolar depression and unipolar depression look almost identical on the surface-both involve deep sadness, fatigue, loss of interest, and trouble sleeping. But treating them the same way can make things worse. In fact, giving someone with bipolar disorder the wrong medication can trigger mania, rapid cycling, or even hospitalization. The difference isn’t just academic-it’s life-changing.
What’s the Real Difference?
Unipolar depression, also called Major Depressive Disorder (MDD), means you experience only depressive episodes. No highs. No energy surges. No periods of reckless spending, grand ideas, or sleepless nights fueled by euphoria. It’s a persistent low. The DSM-5 requires at least five symptoms-including depressed mood or loss of pleasure-for two weeks straight, with no history of mania or hypomania. Bipolar depression is different. It’s not its own disorder. It’s the low phase of bipolar disorder. To be diagnosed with bipolar I or II, you must have had at least one manic or hypomanic episode in your life-even if it was years ago. That’s the line. One manic episode, and your depression is no longer unipolar. It’s bipolar. This isn’t splitting hairs. It’s the difference between taking an SSRI and taking lithium. One can help. The other can hurt.How Doctors Tell Them Apart
Most people with bipolar depression are initially misdiagnosed as having unipolar depression. Studies show up to 40% of people with bipolar disorder spend years being treated for unipolar depression. Why? Because people rarely volunteer that they once went three days without sleep, bought a car on a whim, or felt invincible during a high. They remember the crushing lows. They forget-or minimize-the highs. Clinicians use specific red flags to spot bipolar depression:- Early morning waking (57% of bipolar cases vs. 39% in unipolar)
- Severe morning mood worsening (63% vs. 41%)
- Psychomotor slowing-moving and speaking painfully slowly (68% vs. 42%)
- Psychotic features like delusions or hallucinations during depression (22% vs. 8%)
- Family history of bipolar disorder
- Antidepressants made symptoms worse or triggered mania
- Multiple failed antidepressant trials
Why Treatment Can’t Be the Same
This is where things get dangerous. For unipolar depression, SSRIs like sertraline or escitalopram are standard first-line treatment. About 60-65% of people respond within 8 to 12 weeks. It’s straightforward. For bipolar depression? SSRIs alone are risky. The STEP-BD study found that 76% of bipolar patients on antidepressants without a mood stabilizer experienced mood destabilization-switching into mania, rapid cycling, or mixed states. That’s not a side effect. That’s a treatment failure. Bipolar depression requires mood stabilization first. First-line options include:- Lithium: Proven to reduce depressive episodes by 48% compared to placebo
- Quetiapine: One of the few antipsychotics approved specifically for bipolar depression, with a 58% response rate
- Lurasidone: Also FDA-approved for bipolar depression, with fewer weight gain side effects than others
Therapy: Different Goals, Different Tools
Therapy isn’t one-size-fits-all either. For unipolar depression, Cognitive Behavioral Therapy (CBT) works well. It helps you challenge negative thoughts like “I’m worthless” or “Nothing will ever get better.” You learn to reframe them. For bipolar depression, Interpersonal and Social Rhythm Therapy (IPSRT) is more effective. Why? Because stability is everything. IPSRT trains you to keep your sleep, meals, exercise, and social routines consistent. Why? Because disrupted routines trigger episodes. A 2005 study found that people on IPSRT had a 68% remission rate at 12 months-compared to 42% with standard care. It’s not about changing your thoughts. It’s about protecting your rhythm.What Happens When You Get It Wrong
Misdiagnosis isn’t just a mistake-it’s a cascade of harm. A 2017 study found that people misdiagnosed with unipolar depression when they actually had bipolar disorder spent an average of 8.2 years on the wrong treatment. During that time, 63% were hospitalized due to antidepressant-induced mania. One Reddit user shared: “I was on Prozac for seven years. I went from two episodes a year to twelve. My psychiatrist didn’t notice the hypomania until I nearly lost my job.” The financial cost is just as heavy. Misdiagnosed bipolar patients spend $13,247 more per year on healthcare due to extra hospital visits, ER trips, and medication switches. On the flip side, getting the right diagnosis leads to real improvement. A 2022 survey by the Depression and Bipolar Support Alliance found that people on appropriate treatment saw a 52% drop in hospitalizations and a 47% boost in work performance.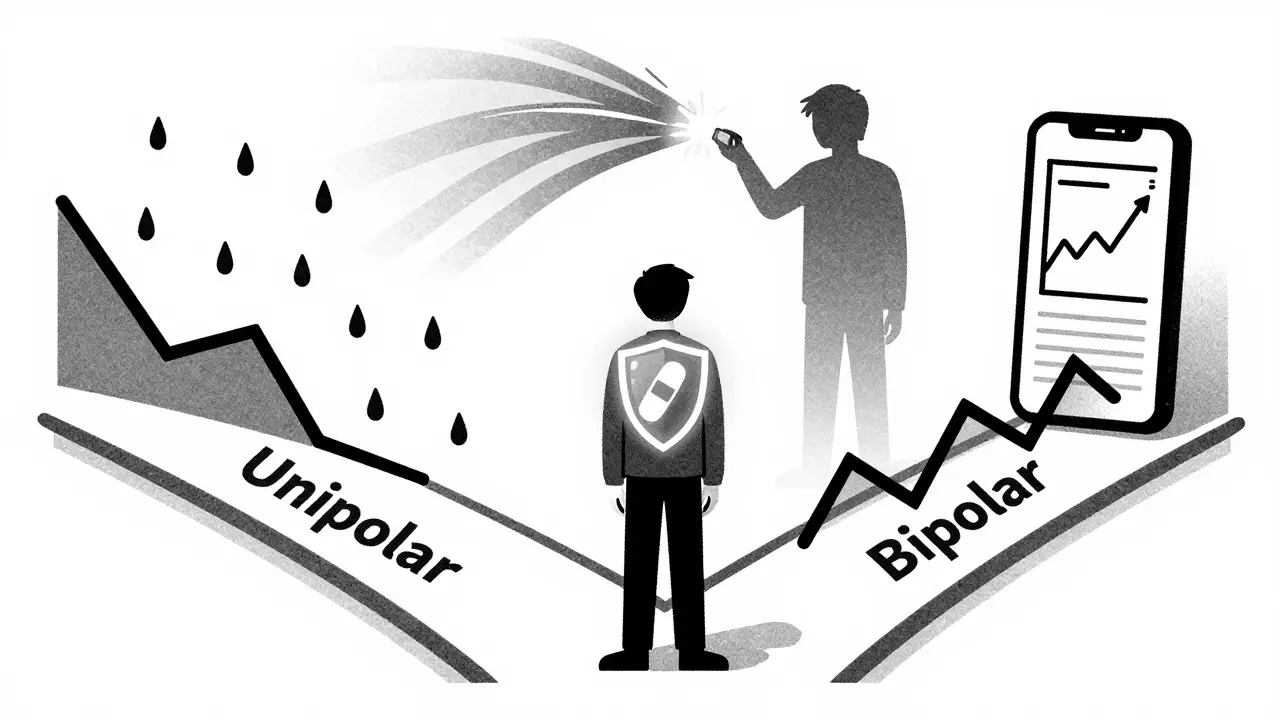
Is There a Spectrum? The Debate
Some experts argue that unipolar and bipolar depression exist on a spectrum. Genetic studies show a strong link-bipolar disorder and major depression share 72% of their genetic risk factors. Some people with recurrent unipolar depression eventually develop hypomania. About 15-20% do, according to researchers like Kay Redfield Jamison. But the DSM-5 keeps them separate. Why? Because treatment decisions depend on clear boundaries. You don’t treat a broken leg the same way you treat a dislocated shoulder-even if both hurt. The DSM-5-TR (2022) added a “with mixed features” specifier for depression. That’s a step toward acknowledging overlap. But the core rule remains: if you’ve ever had mania, your depression is bipolar.What You Should Do
If you’ve been diagnosed with unipolar depression and:- Antidepressants didn’t work-or made things worse
- You have a family history of bipolar disorder
- You’ve had periods of high energy, impulsivity, or reduced need for sleep
- You’ve had more than two failed antidepressant trials
What’s Next?
Research is moving fast. A 2023 Lancet study identified a 12-gene pattern that can distinguish bipolar from unipolar depression with 83% accuracy. Smartphones are being used to track sleep, speech patterns, and typing speed to detect early mood shifts before they become episodes. New drugs like cariprazine and esketamine are expanding options. But the most powerful tool remains accurate diagnosis. Until we can test for it with a blood sample, the best predictor is your history-and your honesty. Don’t let the label define you. But do let it guide your treatment. Because the right diagnosis doesn’t just change your medication. It changes your life.Can you have bipolar depression without ever having mania?
No. By definition, bipolar depression only occurs in people who have had at least one manic or hypomanic episode in their lifetime. If you’ve never had mania or hypomania, your depression is classified as unipolar, even if your symptoms feel severe. Some people forget or minimize past high episodes-especially if they were mild or occurred decades ago. That’s why doctors ask about family history and past behavior patterns.
Are antidepressants always bad for bipolar depression?
Not always, but they’re risky as a standalone treatment. Antidepressants can trigger mania, rapid cycling, or mixed episodes in people with bipolar disorder. The safest approach is to stabilize mood first with lithium, quetiapine, or lurasidone. Only after stability is achieved-and with close monitoring-might an antidepressant be added cautiously, always paired with a mood stabilizer. Never start an antidepressant alone if bipolar disorder is suspected.
How long does it take to get the right diagnosis?
On average, it takes 8 to 10 years for someone with bipolar disorder to receive the correct diagnosis. Many see multiple doctors, try several medications, and get misdiagnosed with anxiety, personality disorder, or unipolar depression first. This delay happens because people don’t report manic symptoms-they’re embarrassed, don’t realize it’s abnormal, or think it’s just “being productive.” The key is to track your mood patterns and share any history of unusual energy, impulsivity, or sleep changes with your clinician.
Can bipolar depression turn into unipolar depression?
No. Once you’ve had a manic or hypomanic episode, your diagnosis is bipolar disorder, even if you haven’t had a high episode in years. The condition doesn’t “turn into” unipolar depression. However, some people with bipolar disorder may go long periods with only depressive episodes, especially with effective treatment. That doesn’t change the diagnosis-it just means the treatment is working.
What should I ask my doctor if I suspect I have bipolar depression?
Ask: “Have I ever had a period where I felt unusually energetic, impulsive, or irritable-even if it didn’t last long?” “Did I ever go days without sleep and still feel fine?” “Have I ever made big financial or relationship decisions I now regret?” “Has anyone in my family been diagnosed with bipolar disorder?” “Have antidepressants ever made me feel worse or more agitated?” These questions help uncover hidden mania. Don’t be afraid to bring up the possibility of bipolar disorder yourself.

Comments
Jamie Hooper
bro i was on sertraline for 5 years and thought i was just 'a really sad person'... then one day i bought a motorcycle, quit my job, and flew to thailand to 'find myself'... turned out i was hypomanic. my doc never asked. no one ever asks. now im on lithium and actually sleep at night. thanks for this post.
January 24, 2026 AT 05:44
Husain Atther
This is a well-structured and clinically accurate overview of a critical distinction in psychiatric care. The emphasis on differential diagnosis and the risks of antidepressant monotherapy in bipolar spectrum disorders is both timely and necessary. I appreciate the inclusion of evidence-based tools such as the MDQ and HCL-32, which remain underutilized in primary care settings globally.
January 24, 2026 AT 15:06
Helen Leite
🚨 ALERT 🚨
THEY DON’T WANT YOU TO KNOW THIS 😱
Big Pharma HATES when people find out SSRIs can trigger MANIA 😤
They profit off endless prescriptions 💸
But lithium? Cheap as dirt. No ads. No stock price. 🤫
They’re hiding the truth. I know. I’ve been there. 💔
January 26, 2026 AT 09:14
Izzy Hadala
Given the findings of the STEP-BD study, one must question the prevailing clinical paradigm that prioritizes antidepressant intervention in the absence of mood stabilization. The statistical risk of mood destabilization-76%-is not merely a side effect profile but a systemic failure in diagnostic fidelity. I would posit that the DSM-5’s categorical distinction, while pragmatic, may be insufficient for a dimensional understanding of affective pathology. Further, the genetic overlap of 72% suggests a neurobiological continuum that warrants reconsideration of diagnostic boundaries.
January 27, 2026 AT 07:41
Marlon Mentolaroc
lol i used to be the guy who thought my 3am binge-buying sprees were just 'being productive'. then i realized i’d spent $12k on amazon in 2 weeks and had zero memory of ordering half of it. my therapist said, 'you had a hypomanic episode.' i said, 'but i felt great!' she said, 'so did the credit card companies.'
turns out, 'feeling great' while bankrupt isn’t a personality trait. it’s a diagnosis.
January 27, 2026 AT 20:58
blackbelt security
Consistency saves lives. Sleep. Meals. Routine. Not magic pills. Not affirmations. Just showing up for yourself every day. I used to think depression was in my head. Turns out, it was in my schedule. IPSRT didn’t fix me. It gave me back my structure. And structure? That’s the real treatment.
January 28, 2026 AT 20:45
Patrick Gornik
Let’s be honest: the DSM is a corporate taxonomy masquerading as science. Bipolar vs. unipolar? It’s a linguistic prison built by psychiatrists who need tidy boxes to bill insurance. The truth? We’re all on a spectrum of dysregulated affect-some just have louder highs and longer lows. And the real tragedy isn’t misdiagnosis-it’s that we’ve reduced the soul’s turbulence to a checklist of symptoms and a formulary of pills that make the system run smoother, not the patient feel better.
They call it 'bipolar disorder' like it’s a disease you catch. But what if it’s not a defect? What if it’s an evolutionary mismatch? A brain wired for intensity in a world that rewards mediocrity?
I’m not saying we toss the science. I’m saying we stop pretending the map is the territory. Your mood isn’t a diagnosis. It’s a language. And we’ve forgotten how to listen.
January 29, 2026 AT 04:46
Tommy Sandri
In many non-Western cultures, episodes of elevated mood are often interpreted within spiritual or communal frameworks rather than clinical ones. In parts of South Asia and Africa, hypomanic episodes may be viewed as signs of divine inspiration or ancestral communication. This cultural reframing may explain why individuals in these regions underreport manic symptoms to Western-trained clinicians, mistaking them for spiritually significant experiences rather than pathological ones. The challenge lies in integrating culturally informed narratives with evidence-based diagnostic criteria without pathologizing normal variations in human experience.
January 31, 2026 AT 00:26