Kidney Disease Antacid Safety Checker
This tool helps you determine if an over-the-counter antacid is safe for you based on your kidney function stage and specific medication. Always consult with your nephrologist before making changes to your medication.
When you have kidney disease, even something as simple as taking an antacid for heartburn can be dangerous. Many people don’t realize that over-the-counter antacids like Tums or Milk of Magnesia aren’t just for indigestion-they can seriously affect your kidneys and electrolytes. For people with chronic kidney disease (CKD), these common meds can turn into silent threats, causing high calcium, high magnesium, or even aluminum poisoning. The line between helpful and harmful isn’t clear unless you know the details.
How Antacids Work-And Why They’re Used in Kidney Disease
Antacids were originally designed to neutralize stomach acid. Calcium carbonate, magnesium hydroxide, and aluminum hydroxide react with hydrochloric acid to reduce burning and discomfort. But in people with kidney disease, these same ingredients do something else: they bind to phosphate in the gut. When kidneys fail, they can’t remove excess phosphate from the blood. That buildup leads to weak bones, itchy skin, and dangerous calcification in blood vessels and the heart.
That’s why doctors sometimes use antacids as phosphate binders. Calcium carbonate (Tums) and aluminum hydroxide (Amphojel) form insoluble complexes with dietary phosphate, stopping it from being absorbed. This helps keep serum phosphate levels between 2.7 and 4.6 mg/dL, the target range recommended by KDIGO guidelines for CKD patients. But here’s the catch: these are not safe for everyone, and they’re not meant to be taken long-term without monitoring.
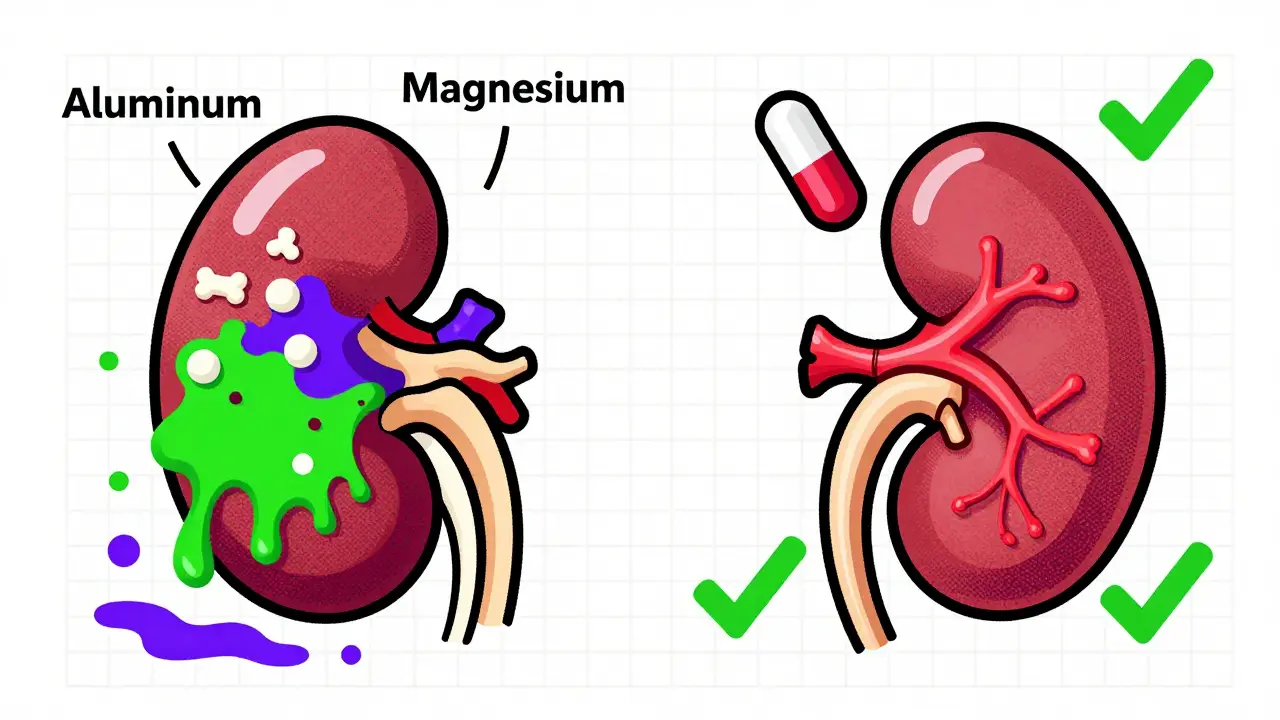
The Hidden Dangers: Aluminum, Calcium, and Magnesium Risks
Not all antacids are created equal when it comes to kidney disease. Each type carries its own set of risks.
Aluminum-based antacids like aluminum hydroxide were once common phosphate binders. But they’re now considered dangerous. Aluminum can build up in the body when kidneys can’t clear it. Levels above 40 mcg/L can cause bone disease; above 60 mcg/L, it can lead to dialysis dementia-memory loss, speech problems, and muscle weakness. The FDA has required warning labels since 1990, and most nephrologists avoid them entirely unless it’s a last-resort, short-term fix. They’re strictly off-limits if your creatinine clearance is below 30 mL/min.
Calcium-based antacids like Tums or calcium citrate are more commonly used. But they’re not harmless. In CKD, your body already struggles to regulate calcium. Too much calcium from antacids can push serum levels above 10.2 mg/dL, increasing the risk of vascular calcification by 30-50%. A 2019 study in the Journal of the American Society of Nephrology found that CKD patients with calcium levels above this threshold had significantly higher rates of heart attacks and strokes. The NEJM reported in 2018 that calcium antacids led to 40% more hypercalcemia cases than non-calcium binders in stage 4 CKD patients.
Magnesium-based antacids like Milk of Magnesia are even riskier. Magnesium is normally excreted by the kidneys. When kidney function drops below 10 mL/min, magnesium builds up. Levels over 4 mg/dL cause muscle weakness and low blood pressure. Above 10 mg/dL, it can stop your breathing or trigger cardiac arrest. The National Kidney Foundation warns that magnesium antacids have caused fatal outcomes in dialysis patients who used them for constipation without knowing the danger.
Prescription Phosphate Binders vs. Over-the-Counter Antacids
Prescription phosphate binders exist for a reason: they’re safer and more effective for long-term use.
- Sevelamer (Renagel): A non-calcium, non-aluminum binder. Reduces phosphate by 25-35% per meal. No risk of aluminum or calcium toxicity. Costs about $2,000-$2,500 per month.
- Lanthanum carbonate (Fosrenol): Similar efficacy to sevelamer. Also avoids calcium and aluminum. Costs $2,500-$3,500 monthly.
- Sucoferric oxyhydroxide (Velphoro): Iron-based. Fewer pills per dose. Costs around $4,000 monthly.
By comparison, generic calcium carbonate costs about $10 a month. That’s why many patients-especially those without good insurance-rely on it. But cost shouldn’t override safety. A 2022 study in the Clinical Journal of the American Society of Nephrology found that 57% of emergency visits related to antacids in CKD patients involved aluminum or magnesium products. Most of these cases were preventable.
Who Should Use What-and When
Not every CKD patient needs the same approach. Your kidney function level determines your risk.
CKD Stage 3 (GFR 30-59 mL/min): Calcium carbonate may be used cautiously. Take it with meals to bind phosphate. Dose: 600-1,200 mg elemental calcium per meal. Monitor serum calcium monthly. Keep it under 10.2 mg/dL. Avoid magnesium and aluminum completely.
CKD Stage 4-5 (GFR under 30 mL/min): Prescription binders only. No OTC antacids for phosphate control. If you need heartburn relief, calcium carbonate may be used occasionally-but only if taken at least 2 hours before or after your prescription binder. Never take it daily. Always check with your nephrologist first.
Also, antacids interfere with other medications. They can reduce absorption of antibiotics, thyroid meds, and seizure drugs like phenytoin by up to 40%. The Cleveland Clinic recommends taking other drugs either one hour before or four hours after an antacid.
What Patients Are Really Experiencing
Real stories show how dangerous this gap in knowledge is.
A 62-year-old woman with CKD stage 4 started taking Tums daily for heartburn. Six months later, her calcium hit 11.2 mg/dL. A CT scan showed new calcium deposits in her arteries. She didn’t know Tums was a phosphate binder.
A man on Reddit shared he used Milk of Magnesia for constipation. His magnesium level spiked to 8.7 mg/dL. He woke up paralyzed in his legs and ended up in the ER.
A 2022 survey by the American Association of Kidney Patients found that 68% of CKD patients couldn’t tell the difference between prescription binders and OTC antacids. Forty-two percent had used antacids without telling their kidney doctor. Only 24% had ever received written instructions about which antacids were safe.

What You Need to Do Right Now
If you have kidney disease and take antacids:
- Stop using aluminum or magnesium antacids immediately. They’re not safe for you.
- If you’re using calcium carbonate daily, talk to your nephrologist. It may be fine in early CKD-but not if your GFR is below 30.
- Ask for a serum calcium, magnesium, and phosphate test. If you’ve been taking antacids for more than a few weeks, you need these checked.
- Learn the difference between your prescription binder and OTC antacids. If you’re unsure, bring the bottle to your next appointment.
- Never take antacids within four hours of other medications. They can make your other drugs less effective.
Also, know the warning signs:
- High calcium: Nausea, confusion, frequent urination, bone pain.
- High magnesium: Muscle weakness, dizziness, low blood pressure, trouble breathing.
- Aluminum toxicity: Memory loss, speech problems, bone pain, anemia.
What’s Changing in 2026
New tools are emerging. Tenapanor (Xphozah), approved in 2023, blocks phosphate absorption differently-without binding. It’s not a phosphate binder at all, just a pill that stops the gut from absorbing it. Early data looks promising, especially for patients who struggle with pill burden.
The NIH is funding a major 5-year study called ASK-D, tracking 5,000 CKD patients to create clearer guidelines. And the FDA is expected to update labeling on OTC antacids by 2025 to explicitly warn kidney patients against using them as phosphate binders.
Meanwhile, clinics are rolling out AI tools that analyze your GFR, diet, lab results, and meds to recommend the safest binder for you. These aren’t science fiction-they’re in use today.
Bottom line: Antacids aren’t harmless. In kidney disease, they’re a medical tool with serious side effects. Don’t assume they’re safe just because they’re on the shelf. Your kidneys can’t protect you from them. Only you-and your doctor-can.
Can I still take Tums if I have kidney disease?
You may be able to take calcium carbonate (Tums) occasionally for heartburn, but only if your kidney function is stage 3 or earlier (GFR above 30 mL/min). Never use it daily as a phosphate binder without your nephrologist’s approval. Avoid it completely if your GFR is below 30, and always take it at least 2 hours apart from your prescription phosphate binder. Monitor your blood calcium levels monthly.
Why are aluminum antacids so dangerous for kidney patients?
Kidneys normally remove aluminum from the body. In advanced kidney disease, aluminum builds up in the blood and tissues. Levels above 40 mcg/L can damage bones; above 60 mcg/L, it can cause brain damage known as dialysis dementia. Symptoms include memory loss, confusion, speech problems, and muscle weakness. The FDA banned long-term use of aluminum antacids in kidney patients decades ago, and they should never be used as a first-line treatment.
Is Milk of Magnesia safe if I have CKD?
No. Milk of Magnesia (magnesium hydroxide) is not safe for anyone with CKD stage 4 or 5 (GFR below 30 mL/min). Magnesium builds up quickly when kidneys fail. Levels above 10 mg/dL can cause respiratory failure, cardiac arrest, or death. Even in stage 3, it’s risky. Always use prescription laxatives instead, and never use it without discussing it with your nephrologist.
What’s the best phosphate binder for someone on a budget?
Calcium carbonate (generic Tums) is the cheapest option at around $10 per month. But it’s only appropriate for early-stage CKD (stage 3) with no signs of vascular calcification. If your GFR is below 30, it’s too risky. For advanced CKD, ask your doctor about generic sevelamer or lanthanum carbonate-some patient assistance programs offer them for under $50/month. Never use antacids as a long-term phosphate binder without supervision.
How do I know if I’m having an antacid-related complication?
Watch for these signs: persistent nausea, confusion, muscle weakness, low blood pressure, trouble breathing, or bone pain. If you’ve been taking antacids and notice any of these, get your blood tested for calcium, magnesium, phosphate, and aluminum levels. Emergency visits for antacid toxicity in CKD patients are common and often preventable. Don’t wait for symptoms to get worse.

