Every year, adverse drug events send over a million people to U.S. emergency rooms and land 125,000 in hospitals - and most of these cases are preventable. This isn’t rare bad luck. It’s systemic. A patient takes a common painkiller with blood thinners. An elderly person gets prescribed five new meds at discharge without anyone checking for interactions. A diabetic misses a meal after an insulin dose change. These aren’t accidents. They’re predictable failures in a system that’s supposed to keep people safe.
What Exactly Is an Adverse Drug Event?
An adverse drug event (ADE) isn’t just a side effect. It’s any harm caused by a medication - whether the drug was used correctly or not. The key distinction? If you take your prescribed dose and get sick, that’s an adverse drug reaction. If a nurse gives you the wrong pill, or a pharmacist misreads the handwriting, or a doctor prescribes a drug that clashes with your other meds - that’s a medication error. Both count as ADEs.
Think of it this way: ADEs include everything from mild rashes to liver failure to death - if the drug was involved. The Institute of Medicine first brought this into the spotlight in 2000 with its report To Err is Human, revealing that medication errors alone caused at least 7,000 deaths each year in U.S. hospitals. Since then, the numbers haven’t dropped. In fact, they’ve grown more complex.
The Five Main Types of Adverse Drug Events
Not all ADEs are the same. Understanding the types helps you spot the risks before they happen.
- Adverse Drug Reactions (ADRs): These happen when your body reacts badly to a drug at normal doses. Think nausea from antibiotics or dizziness from blood pressure meds. About 80% of these are Type A reactions - predictable, dose-related, and often preventable with better monitoring.
- Medication Errors: These are mistakes in prescribing, dispensing, or taking meds. A doctor writes "0.5 mg" but it’s read as "5 mg." A pharmacy gives you the wrong brand. You take your pill twice because you forgot you already did. These are preventable by design - not bad luck.
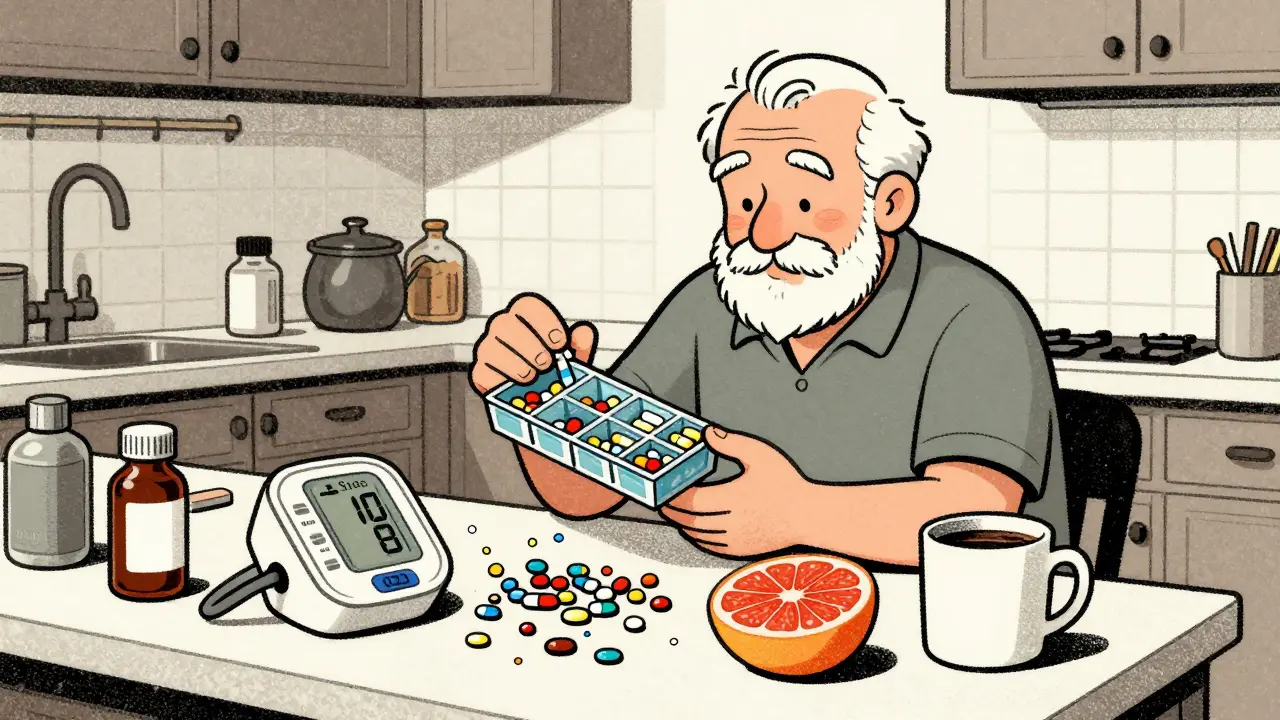
- Drug-Drug Interactions: Two or more drugs mix in your body and create a dangerous effect. Warfarin and certain antibiotics? Big risk for bleeding. Statins and grapefruit juice? Can spike muscle damage. Over 15% of high-risk interactions are flagged by clinical tools - but many still slip through.
- Drug-Food Interactions: Food changes how your body handles drugs. Dairy blocks absorption of some antibiotics. Grapefruit can make cholesterol meds dangerously potent. Even leafy greens can mess with blood thinners by changing vitamin K levels.
- Overdoses: Accidental or intentional. Too much insulin. Taking extra opioids for pain. Mixing alcohol with sedatives. In 2021, synthetic opioids like fentanyl were involved in over 70,000 overdose deaths in the U.S. alone.
The most dangerous ADEs aren’t random. They cluster around three high-risk drug classes: anticoagulants, diabetes medications, and opioids.
Top 3 High-Risk Medications and Why They’re Dangerous
Some drugs are more likely to cause harm - not because they’re bad, but because they’re powerful and have narrow safety margins.
Anticoagulants (like warfarin): These thin your blood to prevent clots. But get the dose wrong, and you bleed internally. Warfarin causes one-third of all ADE-related hospital admissions. Why? It interacts with over 100 other drugs, and your diet (especially vitamin K-rich foods) changes how it works. In 35% of outpatient tests, the blood-thinning level (INR) is outside the safe range - and patients often don’t know it.
Diabetes drugs (especially insulin): Too much insulin? Hypoglycemia. Low blood sugar. Symptoms: shaking, confusion, fainting. In people over 65, 60% of insulin-related ER visits happen because of dosing errors, missed meals, or not adjusting meds after illness. One wrong injection can send someone to the hospital - or worse.
Opioids: Pain relief comes with a deadly trade-off. In 2021, over 107,000 people died from drug overdoses in the U.S. - 70,601 involved synthetic opioids like fentanyl. Even when prescribed correctly, long-term use increases risk of dependence, respiratory depression, and accidental overdose - especially when mixed with alcohol or sleep aids.

How to Prevent Adverse Drug Events - Proven Strategies
You can’t eliminate all risk. But you can cut it dramatically with simple, evidence-backed steps.
- Get a full medication review: Every time you see a new doctor, bring a list of everything you take - including vitamins, supplements, and over-the-counter pills. A 2019 JAMA study showed this cuts ADE risk by 30%. Many patients don’t realize their herbal tea or fish oil interacts with their heart meds.
- Use electronic prescribing: Handwritten prescriptions cause 25% of errors. E-prescribing cuts that by nearly half. It checks for allergies, interactions, and correct doses before the script even leaves the doctor’s computer.
- Ask for medication reconciliation: This is a formal process where your meds are reviewed when you’re admitted to the hospital, transferred between units, or discharged. A 2020 study found it reduces post-discharge ADEs by 47%. Don’t assume your doctor knows what you’re on - show them.
- Get educated on your meds: Know why you’re taking each drug, what it’s supposed to do, and what side effects to watch for. A 2021 Cochrane review found patient education improves adherence by 22% - and better adherence means fewer errors.
- Work with a pharmacist: Pharmacists aren’t just pill dispensers. Medication Therapy Management (MTM) services - offered by many pharmacies - identify an average of 4.2 medication problems per patient. That includes stopping unnecessary drugs, fixing interactions, and adjusting doses. Pharmacist-led anticoagulation clinics cut major bleeding events by 60% compared to standard care.
- Deprescribe when needed: Especially for older adults, taking too many meds is a bigger risk than taking too few. The Veterans Affairs system uses structured deprescribing protocols to stop unnecessary drugs like anticholinergics - and cut ADEs by 40% in seniors.
The Role of Technology and the Future of Safety
Technology is changing how we catch ADEs before they happen.
Hospitals are using real-time dashboards that alert doctors if a patient’s blood levels are drifting out of range - like for warfarin or vancomycin. At Johns Hopkins, AI tools analyze 50+ patient factors - age, kidney function, genetics, current meds - to predict who’s at highest risk for an ADE. Pilot programs cut events by 17%.
Barcode scanning at the bedside ensures the right patient gets the right drug at the right time. The WHO’s global "Medication Without Harm" campaign pushed this tech worldwide - and saw a 18% drop in harm over five years. But the target was 50%. We’re still far behind.
One of the biggest leaps coming? Pharmacogenomics - testing your genes to see how you’ll respond to certain drugs. Right now, only 5% of people get tested. By 2027, that could hit 30%. Imagine knowing before you even take a drug that your body processes it too slowly - and avoiding a dangerous buildup before it starts. That’s not science fiction. It’s already happening in clinics.

Why This Matters to You
If you’re taking even one prescription, you’re at risk. If you’re managing multiple meds for chronic conditions - diabetes, heart disease, depression - your risk is higher. And if you’re over 65, you’re in the highest-risk group. Nearly 40% of ADEs happen in older adults.
But you’re not powerless. You’re the most important person in your own safety chain. Ask questions. Keep a list. Don’t assume your doctor knows everything you’re taking. If something feels off - dizziness, nausea, confusion, bruising - don’t brush it off. Call your pharmacist. They’re trained to spot these things.
The system isn’t perfect. But the tools to fix it exist. What’s missing is awareness - and action.
What’s the difference between an adverse drug reaction and an adverse drug event?
An adverse drug reaction (ADR) is a harmful response to a drug taken correctly at normal doses - like a rash from penicillin. An adverse drug event (ADE) is any injury caused by a drug, whether it was used correctly or not. That includes medication errors, overdoses, and interactions. So all ADRs are ADEs, but not all ADEs are ADRs.
Which medications cause the most adverse drug events?
The top three are anticoagulants (like warfarin), diabetes drugs (especially insulin), and opioids. Warfarin alone causes 33% of all anticoagulant-related ADEs because it has a narrow safety window and interacts with many foods and drugs. Insulin causes over 100,000 emergency visits yearly, mostly in older adults. Opioids led to over 70,000 overdose deaths in 2021.
Can I prevent ADEs on my own?
Yes - and you should. Keep an updated list of all your meds (including supplements and OTC drugs). Bring it to every appointment. Ask your pharmacist to review it. Don’t skip doses or double up without checking. Learn the purpose and side effects of each drug. If something feels wrong, speak up. Your awareness is the first line of defense.
Are electronic prescriptions really safer?
Absolutely. Handwritten prescriptions cause one in four medication errors. Electronic prescribing cuts error rates by 48% by automatically checking for allergies, drug interactions, and correct dosing. It also sends the prescription directly to the pharmacy - no lost papers or misread handwriting.
What should I do if I think I’m having an adverse drug event?
Stop taking the medication if it’s safe to do so - and call your doctor or pharmacist immediately. If symptoms are severe - chest pain, trouble breathing, swelling, confusion, or uncontrolled bleeding - go to the ER. Don’t wait. Bring your full medication list with you. Early action can prevent serious harm.
Is pharmacogenomic testing worth it?
For certain high-risk drugs - like clopidogrel (a blood thinner), certain antidepressants, or chemotherapy agents - yes. Testing can tell you if your body processes the drug too slowly (risking overdose) or too quickly (making it ineffective). Adoption is still low (only 5%), but it’s expected to grow to 30% by 2027. If you’re on long-term meds with known genetic interactions, ask your doctor if testing is right for you.
What Comes Next?
The future of medication safety isn’t about more rules - it’s about smarter systems. AI predicting your risk before you take a pill. Pharmacists embedded in care teams. Genes guiding your dosage. But none of it matters if patients aren’t involved.
You’re not just a recipient of care. You’re a partner in safety. Ask questions. Speak up. Keep your list updated. And if something doesn’t feel right - trust your gut. The system can be improved. But it starts with you.

Comments
Laia Freeman
OMG THIS IS SO REAL!!! I had a friend almost die because her doc prescribed her a new antibiotic and she was already on warfarin-no one checked!!! She ended up in the ER bleeding internally. Like... why do we still let this happen??? 😭
January 28, 2026 AT 16:18
Keith Oliver
Honestly, the entire healthcare system is a charade. You think your doctor cares? They’re paid by volume, not outcomes. They don’t have time to read your 12 meds-you’re just a number. And don’t get me started on pharmacists who can’t even spell 'hypertension.' This isn’t prevention-it’s damage control with a fancy PowerPoint.
January 30, 2026 AT 03:51
ryan Sifontes
they said it was preventable. so why are we still doing it? maybe its all part of the plan. big pharma needs you sick. always.
February 1, 2026 AT 03:48
Laura Arnal
This is so important!! 💪 I work in a clinic and I see this every day. One of my patients just started on insulin and didn’t know grapefruit juice could mess with it-thank god her pharmacist caught it during a med review! 🙌 You guys are NOT powerless. Ask questions. Bring your list. You’re the MVP of your own health!
February 1, 2026 AT 04:18
Jasneet Minhas
The irony is not lost on me. In India, we often can’t afford even one medication, yet here you have an entire system collapsing under the weight of overprescribing. Perhaps the real problem isn’t the drugs-it’s the belief that more is better. 🙄
February 1, 2026 AT 15:57
Eli In
I love how this post doesn’t just blame doctors or patients-it shows how the system fails everyone. My mom’s a diabetic and she’s terrified of insulin because of what happened to her cousin. But she didn’t know she could ask for a pharmacist consult. Now she does. ❤️
February 3, 2026 AT 02:13
Doug Gray
The epistemological rupture in pharmacovigilance is profound. We operate within a hermeneutic framework of biomedical hegemony, where patient agency is commodified as 'adherence'-a performative metric rather than a lived experience. The algorithmic surveillance of INR levels? A techno-bureaucratic mirage. The real issue? The ontological alienation of the patient from their own physiology.
February 4, 2026 AT 12:36
Kristie Horst
I appreciate the effort put into this article. Truly. But I must point out that the phrase 'you’re the most important person in your own safety chain' is a dangerously individualistic framing. When 70% of ADEs occur in elderly patients with cognitive decline, placing the burden on them is not empowerment-it’s negligence. Systemic reform isn’t optional. It’s overdue.
February 4, 2026 AT 23:23
rajaneesh s rajan
I’ve seen this in my dad’s care. He’s 72, on 8 meds. The doctor writes a new script, the pharmacy fills it, no one connects the dots. Then he gets dizzy. We think it’s old age. Turns out it was the new blood pressure pill + his fish oil. Took three visits to figure it out. The system is broken. But hey, at least we got a free pill organizer. 🤷♂️
February 6, 2026 AT 19:33
paul walker
i just started taking metformin and i had no idea it could cause vitamin b12 deficiency. my dr never mentioned it. thanks for the heads up! gonna ask my pharmacist next time.
February 8, 2026 AT 03:44
Alex Flores Gomez
You know what’s wild? The fact that we still use handwritten scripts in 2025. It’s like using a fax machine to order pizza. E-prescribing isn’t 'nice to have'-it’s basic hygiene. And if your doctor still uses scribbles, fire them. Seriously. Your life isn’t a game of Mad Libs.
February 9, 2026 AT 22:12